Pharmaceutical Competition: How Generic Drugs Enter the Market and Change Prices
When we talk about pharmaceutical competition, the process by which new drug makers challenge brand-name manufacturers to lower prices and increase access. Also known as drug market rivalry, it’s what turns a $1,000 monthly pill into a $10 generic version—sometimes in just months. This isn’t just business—it’s personal. If you’re on a chronic medication, this competition could mean the difference between sticking with your treatment or skipping doses because you can’t afford it.
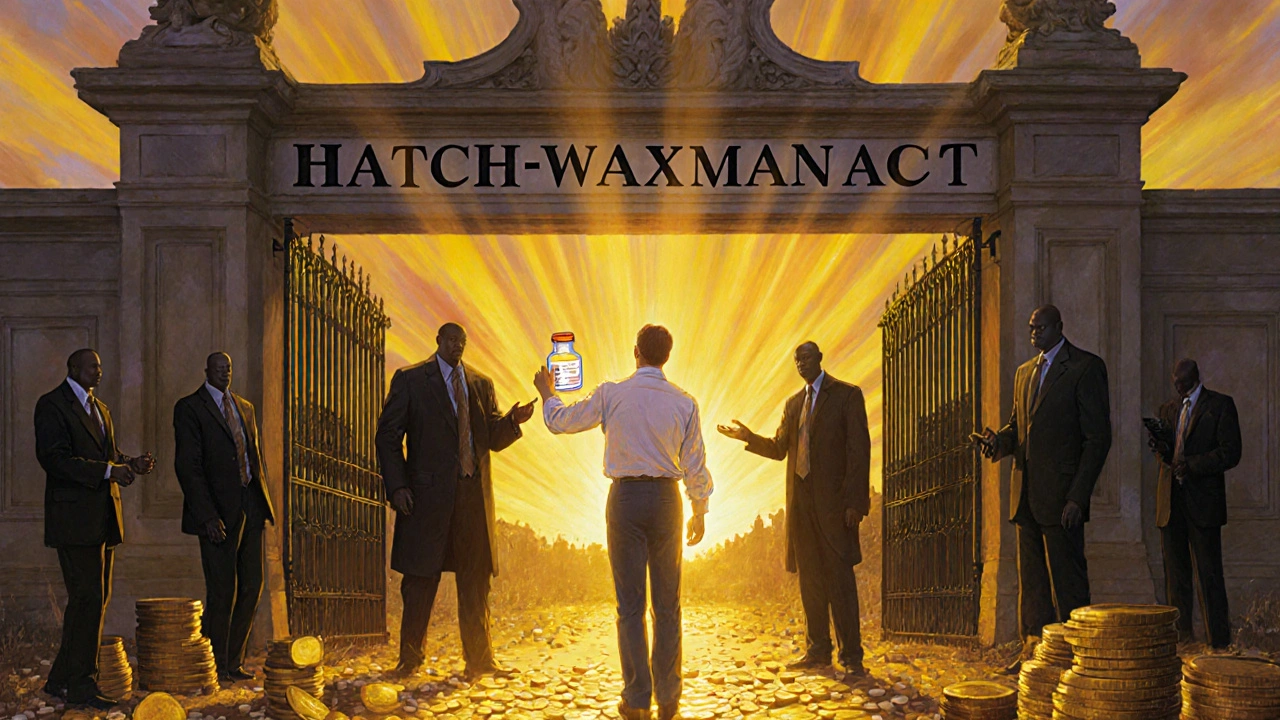
Generic drug entry, when a cheaper version of a brand-name drug hits the market after patent protection ends doesn’t happen automatically. It’s a race between drug companies, lawyers, and regulators. The Hatch-Waxman Act, a 1984 U.S. law that balances innovation with affordability by letting generics enter after patents expire created the pathway, but companies still find ways to delay it—like filing lawsuits, tweaking formulas slightly, or paying generic makers to wait. These delays can cost patients billions. Meanwhile, the FDA generic approval, the process where the FDA reviews and approves generic versions to ensure they work the same as the brand can take anywhere from a few months to over two years, depending on how clean the application is and whether the FDA has backlog.
Patent expiration, the moment a drug’s legal monopoly ends and others can legally copy it is the starting gun. But even after that, the first generic maker often gets a 180-day exclusivity window—meaning they’re the only one allowed to sell it for half a year. That’s why you might see one cheap version appear, then suddenly three more pop up all at once. It’s not magic. It’s strategy.
What you’ll find below isn’t just theory. These are real stories from people who’ve watched drug prices drop—or stayed stuck with high costs because competition was blocked. You’ll see how companies predict when generics will launch, what the FDA actually looks for during review, and how legal loopholes keep prices high even after patents expire. Some posts break down the exact timeline of approval. Others show you how to track when your drug might go generic. There’s even one that explains how AI is now being used to guess when a drug will face competition, before the lawyers even file their papers.
This isn’t about pharmaceuticals as abstract industry terms. It’s about your prescriptions, your co-pays, and whether you can keep taking your medicine next month. The system is complex, but you don’t need to understand every rule to know what matters: competition lowers prices. And knowing how it works helps you fight for better access.
Antitrust Laws and Competition Issues in Generic Pharmaceutical Markets
Antitrust laws in the generic drug market aim to stop big pharma from blocking cheaper alternatives through pay-for-delay deals, patent manipulation, and product hopping. These tactics raise prices and hurt patients - but enforcement is evolving globally.