Generic Medication Effectiveness: Do Cheap Drugs Really Work?
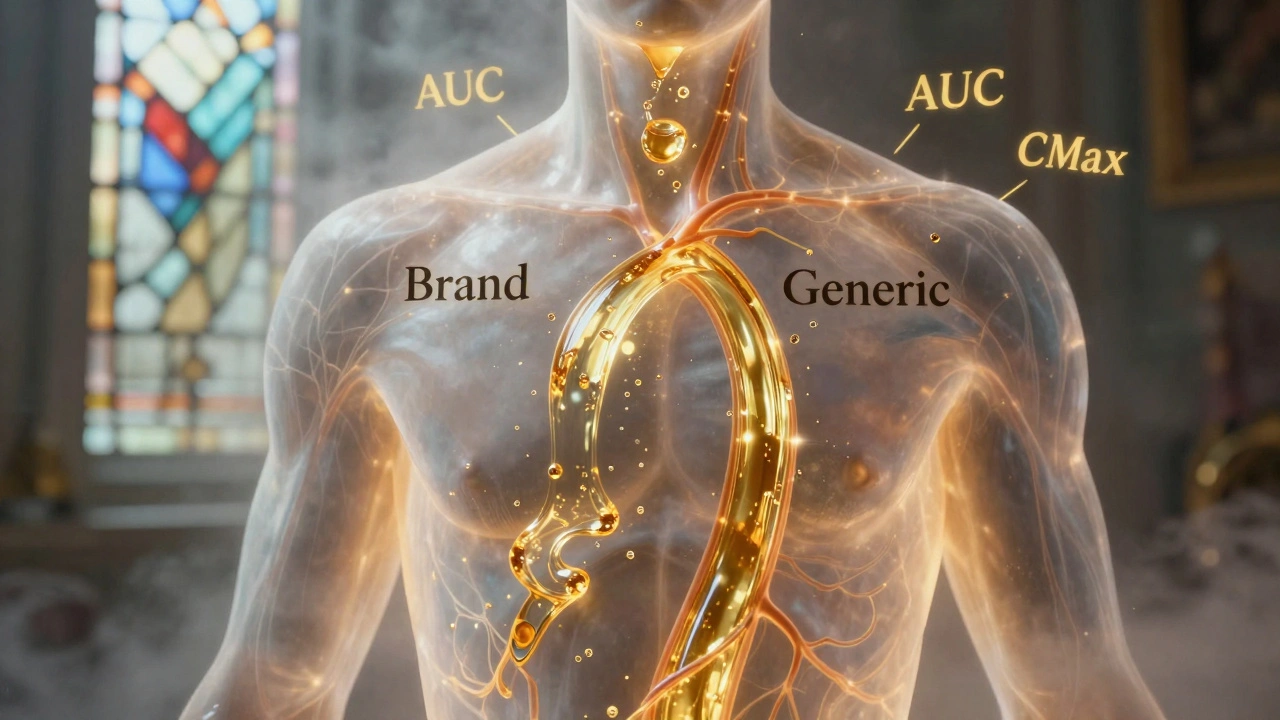
When you pick up a generic medication, a copy of a brand-name drug approved by the FDA after the original patent expires. Also known as generic drugs, it contains the same active ingredient, strength, and dosage form as the brand version—but often costs 80% less. Many people assume cheaper means weaker, but that’s not how the system works. The FDA requires generic medication effectiveness to match the brand-name drug in how fast it’s absorbed, how much enters your bloodstream, and how well it treats your condition. This isn’t guesswork—it’s science, tested in real people under strict rules.
What makes a generic drug work? It’s not the color, shape, or filler. It’s the active ingredient, the component that actually treats your illness. Whether it’s metformin for diabetes or lisinopril for blood pressure, the molecule in your generic pill is identical to the one in the brand. The difference? The inactive ingredients—things like dyes, binders, or coatings. These don’t treat your condition, but they can affect how the pill breaks down in your stomach. For most people, this doesn’t matter. But for those with rare allergies or absorption issues, even small changes can cause noticeable differences. That’s why some patients report feeling different on generics—not because the drug failed, but because their body reacted to something else in the pill.
Here’s what the data shows: over 90% of prescriptions filled in the U.S. are generics, and they save patients and the healthcare system billions every year. Studies tracking outcomes—like hospital visits, blood pressure control, or blood sugar levels—find no meaningful difference between brand and generic versions for the vast majority of conditions. The FDA doesn’t approve generics based on promises. It requires bioequivalence studies proving the generic delivers the same amount of medicine into your blood at the same speed as the brand. If it doesn’t pass, it doesn’t get approved. There’s no loophole.
So why do some people still doubt generics? Partly because of marketing. Brand-name companies spend millions convincing you their version is superior. Partly because of rare cases where switching between different generic manufacturers causes minor fluctuations—especially with drugs like warfarin or thyroid meds, where tiny changes matter. But these aren’t failures of generics—they’re reminders that some medications need closer monitoring, regardless of price tag.
What you’re really looking for isn’t brand or generic—it’s consistency. Stick with the same generic manufacturer if you notice a difference. Ask your pharmacist if your refill switched suppliers. And know this: if your doctor prescribes a brand-name drug with "dispense as written" on the script, it’s usually because of a known sensitivity—not because generics are less effective.
Below, you’ll find real stories, hard numbers, and breakdowns of how generics are tested, why some drugs still lack generic versions, and how to spot the ones that work just as well—without paying extra.
Generic Absorption Rates: How They Must Match Brand Drugs to Be Safe and Effective
Generic drugs must match brand-name absorption rates within strict 80-125% limits to be approved. Science shows they’re nearly identical in effectiveness - with only 3-5% average differences. Learn how bioequivalence works and why generics are safe.