Why Your Eczema Won’t Go Away
Most people think eczema is just dry, itchy skin. But if you’ve had it for years, you know it’s more than that. It’s the sleepless nights from scratching. The red, cracked patches that flare up out of nowhere. The expensive creams that barely help. And the frustration when doctors say, "Just moisturize more."
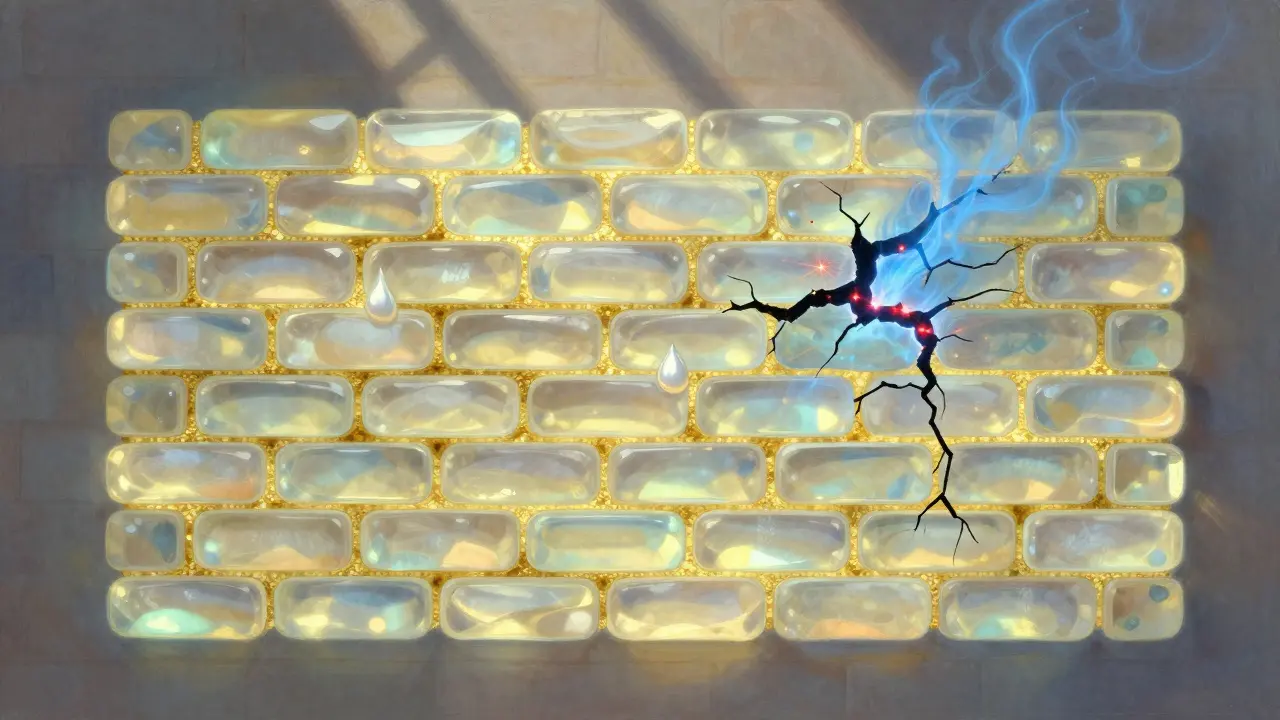
The truth? Chronic eczema-usually called atopic dermatitis-isn’t just a surface problem. It starts with a broken skin barrier. Your skin’s outer layer is supposed to act like a brick wall, with cells (bricks) held together by lipids (mortar). In eczema, that mortar is missing. Ceramides, cholesterol, and fatty acids-the building blocks-are gone. That’s why water escapes (called transepidermal water loss), and irritants, bacteria, and allergens slip in. This isn’t a side effect. It’s the root cause.
A 2025 study in Frontiers in Immunology found that in high-risk babies, this barrier breaks down 3 to 6 months before the first rash appears. That means the damage starts before you even notice it. And if you have a filaggrin gene mutation (which about half of moderate to severe cases do), your body can’t make enough of the protein that holds the bricks together. Your skin is literally falling apart from the inside.
What Actually Repairs the Barrier (And What Doesn’t)
Not all moisturizers are created equal. Vaseline? It seals in moisture but doesn’t fix the broken mortar. Aloe vera gel? Hydrates but doesn’t rebuild. Even many "dermatologist-recommended" creams are just water with a little oil.
Real barrier repair needs the right lipids in the right ratios. Think of it like fixing a wall-you don’t just slap on paint. You need the same materials that were there originally. That’s why products with a 1:1:1 ratio of ceramides, cholesterol, and free fatty acids work. Clinical trials show these restore the barrier 87% of the time, compared to just 52% with regular lotions.
Look for these numbers on the label:
- Ceramides: 3% to 5%
- Cholesterol: 2% to 4%
- Free fatty acids: 1% to 3%
And check the pH. Your skin’s natural pH is 4.5 to 5.5. If the product is too alkaline (like soap-based cleansers), it shuts down the enzymes that make ceramides. The best barrier creams are pH 5.0 to 5.5. That’s why CeraVe, EpiCeram, and similar products work-they’re designed to match your skin’s chemistry.
A 2023 head-to-head trial found ceramide-based creams reduced water loss by 42.7% after 28 days. Petrolatum-based ones? Only 28.3%. That’s a huge difference when you’re trying to stop flares.
The Top Triggers You’re Probably Ignoring
Stress, dust mites, pollen-those are the usual suspects. But here’s what most people miss:
- Hot showers: Water above 100°F strips away the last of your skin’s natural oils. Even 5 minutes is enough to trigger a flare.
- Harsh soaps: Cleansers with sodium lauryl sulfate (SLS) dissolve lipids. Switch to a soap-free, fragrance-free cleanser like Cetaphil or Vanicream.
- Dry air: Especially in winter, indoor heating drops humidity below 30%. Use a humidifier in your bedroom-aim for 40-50%.
- Sweat: Salt and bacteria in sweat irritate broken skin. Shower within 15 minutes after exercise. Pat dry-don’t rub.
- Wool and synthetic fabrics: Scratchy textures rub against inflamed skin. Stick to cotton, bamboo, or silk.
- Overwashing: Washing your face or hands more than twice a day? You’re stripping your barrier. Use water alone when you can.
One Reddit user, u/EczemaWarrior, tracked their triggers for 6 months. They cut out hot showers, switched to cotton pajamas, and started using a humidifier. Their flares dropped from 4 times a week to once a month.

How to Stop the Itch-Without Steroids
Itch is the worst part. It’s not just annoying-it’s a reflex loop. Scratch → inflammation → more itch → more scratch. And you don’t even realize you’re doing it while sleeping.
Here’s what works:
- Cool compresses: Dampen a clean cloth with cool (not icy) water. Hold it on the itch for 5 minutes. It blocks the itch signal to your brain.
- Wet wrap therapy: After applying your barrier cream, put on a damp cotton shirt or bandage, then cover with dry clothing. This traps moisture and reduces scratching. Do it for 1-2 hours or overnight.
- Antihistamines: Only help if itch is allergy-driven. Most eczema itch isn’t. But diphenhydramine (Benadryl) at night can help you sleep.
- Topical JAK inhibitors: Ruxolitinib cream (Opzelura) blocks itch signals at the nerve level. FDA-approved for eczema. Works in days, not weeks.
- Mindful distraction: A 2024 study found that 10 minutes of focused breathing or squeezing a stress ball reduced scratching by 60% in adults.
Don’t rely on steroids long-term. Betamethasone 0.1% reduces itch fast, but it thins your skin by 15-20% over time. Pimecrolimus (Elidel) doesn’t thin skin, but it takes longer. For chronic cases, barrier repair + JAK inhibitor is the new gold standard.
How to Use Barrier Creams Right
Using the right cream won’t help if you’re using it wrong. Here’s the exact routine:
- Bath or shower: Use lukewarm water (under 100°F) for 5-10 minutes max. No scrubbing.
- Pat dry: Gently blot skin with a towel. Leave it slightly damp.
- Apply cream within 3 minutes: This locks in 35% more moisture than waiting. Use 2 fingertip units (about a teaspoon) per arm or leg.
- Apply twice daily: Morning and night. No exceptions.
- Wait 15 minutes before steroid: If you use a prescription steroid, apply the barrier cream first. Wait 15 minutes. Then apply the steroid. Mixing them reduces effectiveness.
Most people quit because the cream feels greasy. That’s normal. It’s not supposed to feel like a light lotion. It’s medicine. Stick with it for 4 weeks. That’s how long it takes to rebuild the barrier. One study showed 92% of users saw real improvement only after 28 days of daily use.

When Barrier Repair Alone Isn’t Enough
Here’s the hard truth: barrier repair works for 60-70% of people. But for those with severe filaggrin mutations, it’s not enough. Their TEWL (water loss) can hit 45 g/m²/h-more than triple the normal rate. No cream can fully fix that.
If you’ve been using ceramide creams for 12 weeks with no change, talk to your dermatologist about:
- JAK inhibitors: Oral or topical drugs like upadacitinib or ruxolitinib that calm the immune system at the source.
- Biologics: Dupilumab (Dupixent) blocks the key inflammation signal (IL-4/IL-13) driving eczema. Shown to reduce flares by 75% in severe cases.
- Phototherapy: UVB light therapy reduces inflammation and bacteria. Safe for long-term use.
Dr. Emma Guttman-Yassky’s lab found that barrier repair alone normalizes 78% of the abnormal genes in eczema skin. But if inflammation is already running wild, you need to shut that down too. It’s not either/or-it’s both.
Cost, Coverage, and What’s Coming Next
Good barrier creams cost $25-$35 for 200g. Basic moisturizers? $10. That’s why so many people stop. Insurance covers prescription barrier products like EpiCeram 80% of the time-but only if your doctor prescribes them. Over-the-counter ones? Often not covered.
But things are changing. The FDA now requires all barrier repair products to prove they reduce TEWL in clinical trials. That’s raising quality-and prices. By 2027, EU rules will require 30% of ingredients to be biodegradable. That means fewer silicones, more plant-based oils.
On the horizon: personalized eczema care. Companies like Dermavant are using 23andMe data to match patients with ceramide blends based on their filaggrin mutation. Early results show 85% accuracy in predicting which cream will work best. Imagine knowing exactly which product your skin needs-before you buy it.
Real People, Real Results
One 7-year-old with severe eczema was using steroid creams daily. After switching to daily ceramide therapy and wet wraps, their steroid use dropped 80% in 4 months. Their skin cleared. They stopped scratching at night. They started sleeping through the night.
A woman in her 50s, tired of burning sensations from creams, switched to a pH-balanced ceramide cream. Her stinging stopped. Her flares went from weekly to once every 6 weeks.
These aren’t miracles. They’re science. You don’t need to live with cracked, itchy skin. The barrier can heal. The itch can fade. But it takes the right approach-consistently applied.
Can I use barrier repair cream with topical steroids?
Yes, but not at the same time. Apply your barrier cream first. Wait 15 minutes. Then apply the steroid. Mixing them reduces how well both work. This is recommended by the National Eczema Association and backed by clinical studies.
Why does my barrier cream sting when I apply it?
Stinging usually means your skin is cracked or inflamed. Barrier creams with ceramides often have a slightly acidic pH (5.0-5.5) to activate repair enzymes. That can burn on open skin. It’s not an allergy-it’s irritation. Try applying a thin layer of petrolatum first to protect the worst areas, then use the ceramide cream around it. The sting usually fades after 3-5 days as your skin heals.
How long until I see results from barrier repair?
Most people notice less dryness and fewer flares after 2 weeks. But real barrier repair-measurable reduction in water loss and improved skin thickness-takes 4 to 6 weeks. A 2023 NIH study found 92% compliance was needed for significant results. Don’t quit if you don’t see change right away.
Are expensive barrier creams worth it?
Yes-if they contain the right lipids in the right ratios. A $30 cream with 3% ceramides, 2% cholesterol, and 1% fatty acids will work better than a $10 cream with just glycerin and mineral oil. Look at the ingredient list, not the price tag. Brands like CeraVe, EpiCeram, and TriCeram have published clinical data. Cheaper brands often don’t.
Can I outgrow chronic eczema?
Many children do-about 60% by age 12. But for adults, it’s usually lifelong. That doesn’t mean you’re stuck with flares. With consistent barrier repair and trigger management, most adults can live with minimal symptoms. It’s not about curing it-it’s about controlling it.
Solomon Ahonsi
February 1, 2026 AT 18:40George Firican
February 3, 2026 AT 16:41Matt W
February 5, 2026 AT 05:13Anthony Massirman
February 7, 2026 AT 02:39Brittany Marioni
February 7, 2026 AT 12:31Dan Pearson
February 9, 2026 AT 01:27Marc Durocher
February 9, 2026 AT 22:30larry keenan
February 10, 2026 AT 10:04Nick Flake
February 12, 2026 AT 00:06Akhona Myeki
February 12, 2026 AT 01:52Brett MacDonald
February 13, 2026 AT 14:01