What You Need to Know About Organ Rejection
If you or someone you know has undergone an organ transplant, the term "organ rejection" might sound scary but understanding it can make a big difference. Organ rejection happens when your body's immune system attacks the new organ because it views it as a foreign invader. This response is natural but can be managed with the right care and medications.
How Does Organ Rejection Happen?
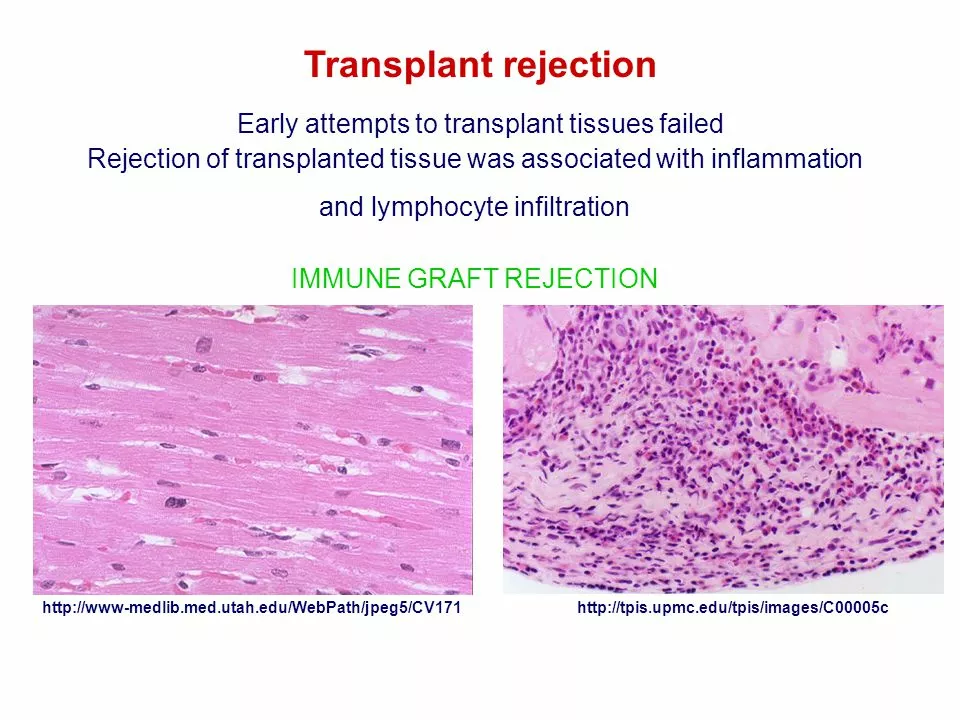
Your immune system is designed to protect you from harmful invaders like viruses and bacteria. When a new organ comes from a donor, the immune system identifies the donor's cells as foreign. It then activates defense mechanisms to attack the new organ, which can lead to damage or failure if not controlled. There are three main types of rejection: hyperacute, acute, and chronic. Hyperacute happens almost immediately, acute occurs within weeks or months, and chronic develops over a long term. Recognizing these types helps doctors find the right treatment quickly.
Signs to Watch For and How to Prevent Rejection
Knowing the signs of rejection gives you a head start in getting help. Common symptoms include fever, pain or swelling near the transplant site, flu-like symptoms, and organ-specific problems like reduced kidney function or breathing issues if it's a lung transplant. Don't ignore these signs—they're signals that your body might be fighting the transplant.
The good news is that with modern medicine, rejection is often manageable. Patients usually take immunosuppressants—drugs that dial down the immune system's attack mode to tolerate the new organ. Sticking to your medication schedule is crucial; skipping doses can increase rejection risks. Also, regular checkups let your healthcare team catch subtle changes early.
Beyond meds, a healthy lifestyle supports your transplant. Eating balanced meals, avoiding infections, and keeping stress low can help your immune system stay in balance. Remember, your transplant is a team effort between you and your medical providers.
Organ Rejection and Ethnicity: The Impact of Genetic Factors
In my recent research, I've come across the fascinating topic of organ rejection and ethnicity, specifically focusing on the impact of genetic factors. It's intriguing to see how genetic variations among different ethnic groups can affect organ transplant outcomes. For instance, certain populations may experience higher rates of organ rejection due to a lack of well-matched donors within their ethnic group. This highlights the importance of increasing organ donor awareness and participation among diverse populations to ensure the best possible outcomes for all patients in need of transplants. Overall, understanding the role of genetic factors in organ rejection is crucial for improving transplantation success rates and saving more lives.