Opioid Dose Converter
This tool converts opioid doses to morphine milligram equivalents (MME) to help you understand your actual medication dose. The CDC recommends not exceeding 50 MME/day without careful medical reassessment.
Your dose converts to 0 MME
Note: MME helps compare different opioids by standardizing to morphine's potency
The CDC recommends not exceeding 50 MME/day without careful reassessment. Higher doses significantly increase overdose risk.
If you've been off opioids for more than 7 days, your tolerance is significantly reduced. Starting at 1/10 of your previous dose is critical to avoid overdose.
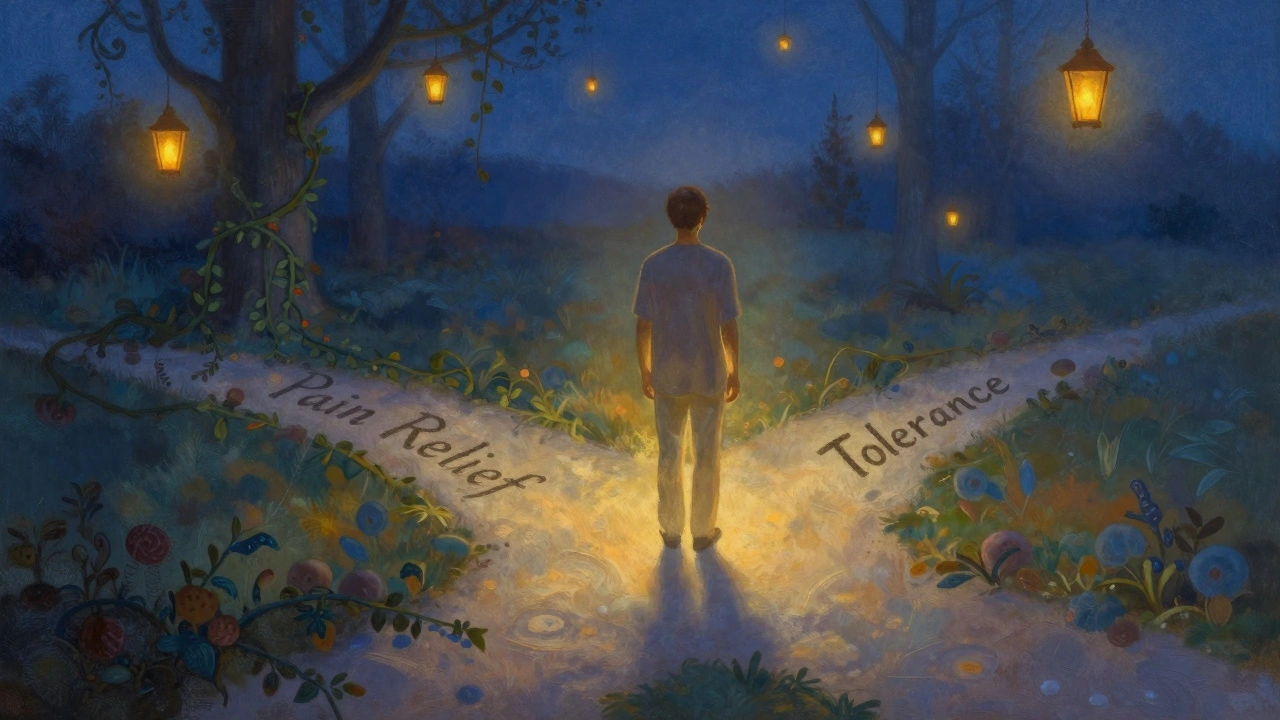
When you first start taking opioids for pain, they work. You feel relief. But over time, that same dose doesn’t do the same thing. You need more. Not because your pain got worse - but because your body changed. This isn’t weakness. It’s biology. And it’s called opioid tolerance.
What Exactly Is Opioid Tolerance?
Opioid tolerance happens when your body gets used to the drug. The brain and nervous system adapt. The receptors that opioids bind to - mainly the mu-opioid receptor, encoded by the OPRM1 gene - start responding less. Over time, they become less sensitive. Some even get pulled inside the cell or reduced in number. That means the same amount of drug no longer triggers the same level of pain relief or euphoria.
This isn’t addiction. It’s not the same as dependence. And it’s not a moral failing. It’s a measurable, predictable physiological response. The U.S. Food and Drug Administration defines it simply: exposure to opioids causes changes that reduce their effects over time. That’s why doctors sometimes have to raise the dose - not because you’re "needing more," but because your body now needs more to get the same result.
Why Does This Happen So Fast for Some People?
Tolerance doesn’t happen the same way for everyone. Some people develop it in weeks. Others stay stable for months. Why? Genetics play a big role. Your body’s metabolism, how your liver breaks down the drug, and even small differences in your opioid receptor structure can change how quickly tolerance builds.
How often you take the drug matters too. Taking opioids daily, even as prescribed, speeds up tolerance. It’s not about how strong the pill is - it’s about how consistently your nervous system is being exposed to it. Studies show that around 30% of people on long-term opioid therapy need higher doses within the first year just to manage the same level of pain.
And it’s not just about pain relief. Tolerance develops at different rates for different effects. You might lose pain control quickly, but still feel the same level of drowsiness or respiratory depression at your original dose. That’s dangerous. It means you could be taking more - thinking you need it for pain - while your breathing is being suppressed at the same level as before.
Tolerance vs. Dependence vs. Addiction
People often mix these up. Let’s clear it up.
Tolerance means you need more of the drug to get the same effect.
Dependence means your body has adjusted to having the drug around. If you stop suddenly, you get withdrawal - sweating, nausea, anxiety, muscle aches. That’s physical adaptation. It doesn’t mean you’re addicted.
Opioid Use Disorder (OUD) is when the drug starts controlling your life. You keep using despite harm - to your health, relationships, job. You might crave it, hide use, or keep taking it even when you know it’s hurting you.
Here’s the key: you can have tolerance and dependence without OUD. Many people on long-term pain meds do. But tolerance is a major stepping stone toward addiction - especially if someone starts chasing the high instead of the pain relief.
The Dangerous Cycle: More Dose, More Risk
When tolerance sets in, the natural response is to take more. That’s human. But with opioids, every increase raises the risk of overdose - especially when the drug’s potency isn’t consistent.
Take fentanyl. It’s 50 to 100 times stronger than morphine. Street drugs laced with it vary wildly - one batch might be 2mg, the next 100mg. Someone with tolerance to prescription oxycodone might take what they think is a normal dose of a street pill - not realizing it’s loaded with fentanyl. That’s how overdose happens.
The CDC reports that in 2022, over 81,000 overdose deaths in the U.S. involved synthetic opioids. Most of those involved people who had developed tolerance to prescription opioids but were now using illicit drugs they couldn’t accurately dose.
And it’s not just street drugs. Even in medical settings, dose escalation without reassessment is risky. The CDC recommends that before increasing opioid doses beyond 50 morphine milligram equivalents (MME) per day, doctors should stop and ask: Is this still helping? Are there safer alternatives?
Tolerance Can Vanish - And That’s Deadly
Here’s the part no one talks about enough: tolerance can disappear.
If you stop taking opioids - whether because you went to rehab, got locked up, took a break, or had surgery - your body forgets how to handle them. Your receptors reset. Your sensitivity returns.
That means if you go back to your old dose - the one you used to take before you stopped - you could overdose. Your body can’t handle it anymore.
Studies show that 74% of fatal overdoses among people recently released from prison happen in the first few weeks. Why? Because they return to their old habits - unaware their tolerance is gone.
The same goes for people in recovery. Sixty-five percent of overdose deaths in recovery involve people who relapse and take their previous dose. They think they can handle it. They can’t.
This is why experts say: if you’ve been abstinent, start with a fraction of your old dose. One-tenth. One-fifth. Don’t guess. Be safe.
What Can Doctors Do About It?
Doctors aren’t blind to this. When tolerance develops, they have tools.
One is opioid rotation. Switching from one opioid to another - say, from oxycodone to hydromorphone - can sometimes restore pain control without increasing the total dose. That’s because tolerance isn’t always complete across all opioids.
Another is combination therapy. Early trials are testing low-dose naltrexone (a drug that blocks opioid receptors) alongside opioids. Early results show it can slow tolerance development by up to 60%. That means patients might stay on lower, safer doses longer.
And yes - blood tests can help. They don’t diagnose tolerance, but they can show if someone is taking what they say they are. Combined with physical exams and symptom tracking, they give doctors a clearer picture.
But the most important tool? Education. Patients need to know: tolerance is normal. It doesn’t mean you’re failing. But it does mean you need to work with your doctor - not push for higher doses on your own.

What Should You Do If You’re on Opioids?
If you’re taking opioids for pain:
- Don’t increase your dose without talking to your doctor.
- Ask: "Is this still working? Are there other options?"
- Track your pain levels and side effects. Bring that to appointments.
- Know your dose in morphine milligram equivalents (MME). Many apps and online calculators can help.
- If you’ve stopped for any reason - even a week - assume your tolerance is lower. Start low if you restart.
If you’re helping someone else:
- Don’t assume they "need more" because they’re asking for it. Tolerance is real - but so is addiction.
- Encourage them to talk to their provider about alternatives: physical therapy, nerve blocks, non-opioid meds like gabapentin or duloxetine.
- If they’re in recovery, remind them: tolerance drops fast. Don’t go back to old habits.
The Bigger Picture: Why This Matters
Opioid tolerance isn’t just a medical footnote. It’s a core driver of the overdose crisis. Every time someone increases their dose because the old one doesn’t work, they edge closer to danger. Every time someone relapses without knowing their tolerance is gone, they risk death.
Research is moving forward. Scientists are studying inflammatory pathways like TLR4 and NLRP3 inflammasomes - and finding drugs that might block tolerance before it starts. The FDA is now pushing for new pain medications designed to avoid tolerance entirely.
But until then, the best protection is knowledge. Understanding that tolerance is normal, predictable, and reversible - and that it’s not a sign of failure, but a signal to pause, reassess, and act safely - could save your life.
Is opioid tolerance the same as addiction?
No. Tolerance means your body needs more of the drug to get the same effect. Addiction - or opioid use disorder - means you keep using despite harm to your health, relationships, or life. You can have tolerance without addiction. But tolerance often leads to addiction if doses keep rising.
Can you develop tolerance to opioids in just a few weeks?
Yes. Some people develop noticeable tolerance within 2-4 weeks of daily use. Genetics, metabolism, and dosage all play a role. It’s not rare - about 30% of patients on long-term opioids need higher doses within the first year.
Why do doctors sometimes switch opioids instead of just increasing the dose?
Because tolerance isn’t always complete across all opioids. Switching from one to another - like from oxycodone to hydromorphone - can restore pain relief without increasing the total daily dose. This is called opioid rotation and is a common strategy when tolerance limits effectiveness.
If I stop taking opioids for a while, will I lose my tolerance?
Yes. Your body resets. If you’ve been off opioids for days or weeks - whether due to rehab, incarceration, or a break - your tolerance drops significantly. Returning to your old dose can cause a fatal overdose. Experts say: if you relapse, start with one-tenth of your previous dose.
Are there new treatments to prevent opioid tolerance?
Yes. Researchers are testing drugs that block inflammatory pathways like TLR4 and NLRP3, which contribute to tolerance. Early trials combining low-dose naltrexone with opioids show up to 60% less dose escalation. The FDA is also encouraging drug developers to create new painkillers that don’t cause tolerance.
What Comes Next?
If you’re on opioids and feel like they’re losing their effect, don’t panic. Don’t self-adjust. Talk to your doctor. Ask about non-opioid options. Ask about rotation. Ask about monitoring.
If you’re in recovery, know this: your tolerance is lower than you think. That’s not a weakness - it’s a fact. Respect it. Start low. Go slow.
Tolerance isn’t a failure. It’s a signal. And how you respond to it - with knowledge, caution, and professional support - makes all the difference between managing pain and risking your life.
Lara Tobin
December 13, 2025 AT 23:37Jamie Clark
December 15, 2025 AT 12:30Harriet Wollaston
December 15, 2025 AT 19:05Lauren Scrima
December 17, 2025 AT 06:59sharon soila
December 18, 2025 AT 19:43Tyrone Marshall
December 18, 2025 AT 22:58Emily Haworth
December 20, 2025 AT 00:52Yatendra S
December 20, 2025 AT 13:57Himmat Singh
December 22, 2025 AT 02:05kevin moranga
December 22, 2025 AT 21:39Alvin Montanez
December 23, 2025 AT 15:32Webster Bull
December 25, 2025 AT 10:04Bruno Janssen
December 26, 2025 AT 11:45Scott Butler
December 27, 2025 AT 02:22Emma Sbarge
December 28, 2025 AT 14:25