Hypoglycemia: Causes, Symptoms, and Treatment Options
When dealing with Hypoglycemia, a condition where blood glucose drops below normal levels, causing a range of physical and mental effects. Also known as low blood sugar, it can strike anyone but shows up most often in people managing Diabetes, a chronic disorder that affects how the body handles glucose. Understanding the link between these two entities helps you spot problems early and act fast.
Why Blood Sugar Can Plummet
Several factors push glucose down. Insulin, the hormone that moves sugar from the bloodstream into cells is a primary driver. Too much insulin—whether from a medication dose, a pancreatic tumor, or a mis‑timed injection—can over‑clear glucose and trigger hypoglycemia. Skipping meals, intense exercise, or drinking alcohol without food also create gaps between supply and demand, especially for those on insulin or insulin‑secretagogues.
Symptoms appear in stages. Early signs include shakiness, sweating, rapid heartbeat, and a sudden urge to eat. If you press on, the brain starves for fuel, leading to confusion, blurred vision, or irritability. Severe episodes can cause seizures, loss of consciousness, or even coma. Recognizing the progression lets you intervene before the situation worsens.
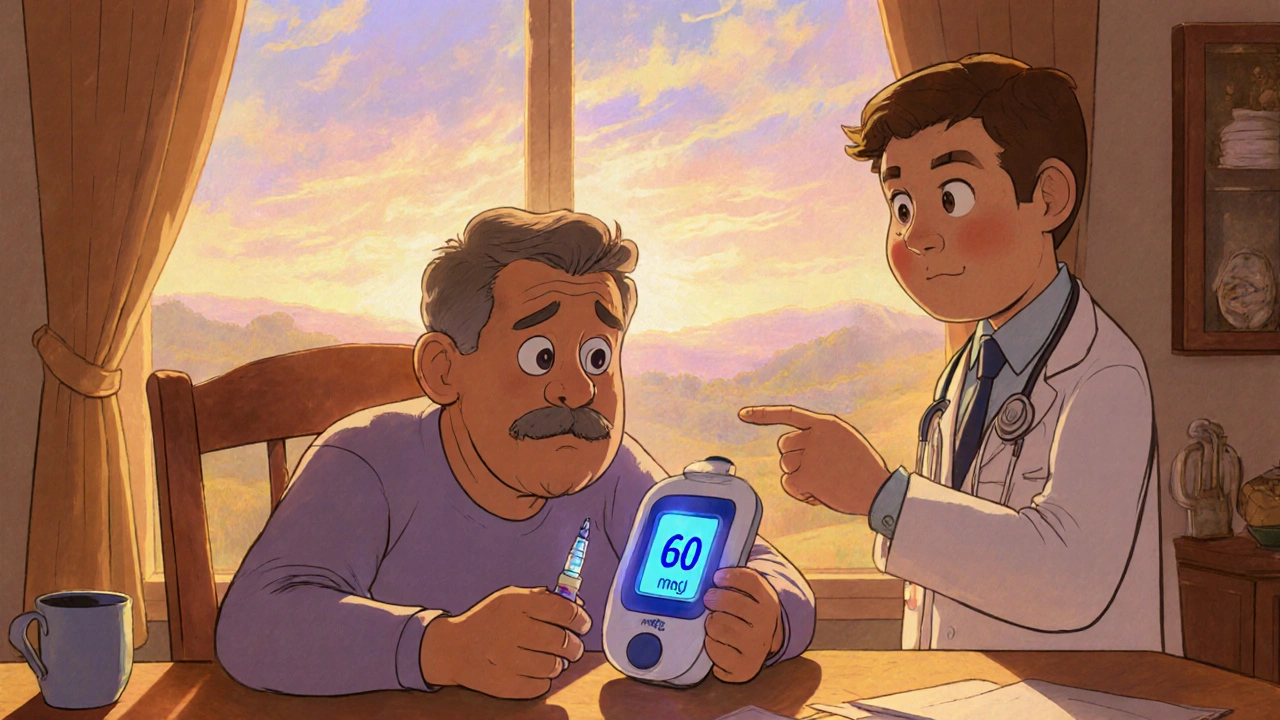
Prevention hinges on routine Glucose Monitoring, regular checks of blood sugar using a meter or continuous sensor. By tracking trends, you can adjust food intake, activity, or medication to keep levels in the safe zone. Many modern devices alert you when readings dip, giving a chance to treat the low before symptoms flare.
When an episode hits, the first move is fast‑acting carbs: glucose tablets, fruit juice, or regular soda. Aim for 15‑20 grams, wait 15 minutes, then re‑check. If you can’t swallow safely—due to confusion or unconsciousness—administer a glucagon injection or nasal spray. Glucagon signals the liver to release stored glucose, acting as a rescue for severe lows.
Beyond emergency steps, long‑term strategies include balanced meals with complex carbs, protein, and healthy fats, plus timing meals around insulin peaks. Working closely with a healthcare provider to fine‑tune medication doses is crucial; small adjustments can prevent recurrent lows. For people without diabetes, investigating underlying causes—like hormonal disorders or medication side effects—is equally important.
Below you’ll find a curated set of articles that dive deeper into medication comparisons, managing related conditions, and lifestyle tweaks that help keep blood sugar stable. Whether you’re looking for drug‑specific guidance or broader health tips, the resources here are organized to give you practical takeaways for avoiding and handling hypoglycemia.
Insulin Therapy Side Effects: Managing Hypoglycemia & Weight Gain
Learn why insulin therapy can cause hypoglycemia and weight gain, how to recognize and treat lows, and practical steps to keep weight in check.