Linezolid Mechanism Quiz
Linezolid is an oxazolidinone antibiotic that targets the bacterial protein‑synthesis machinery. Approved in 2000, it quickly became a go‑to option for multidrug‑resistant Gram‑positive infections such as MRSA and VRE. Its unique binding site on the 50S ribosomal subunit sets it apart from older classes like beta‑lactams or glycopeptides.
Why Linezolid Matters in Modern Therapy
Clinicians reach for linezolid when oral therapy is needed, when patients can’t tolerate intravenous drugs, or when the pathogen shows resistance to first‑line agents. Its excellent bioavailability (>90% after oral dosing) means you can switch from IV to pills without losing coverage - a key advantage in outpatient settings.
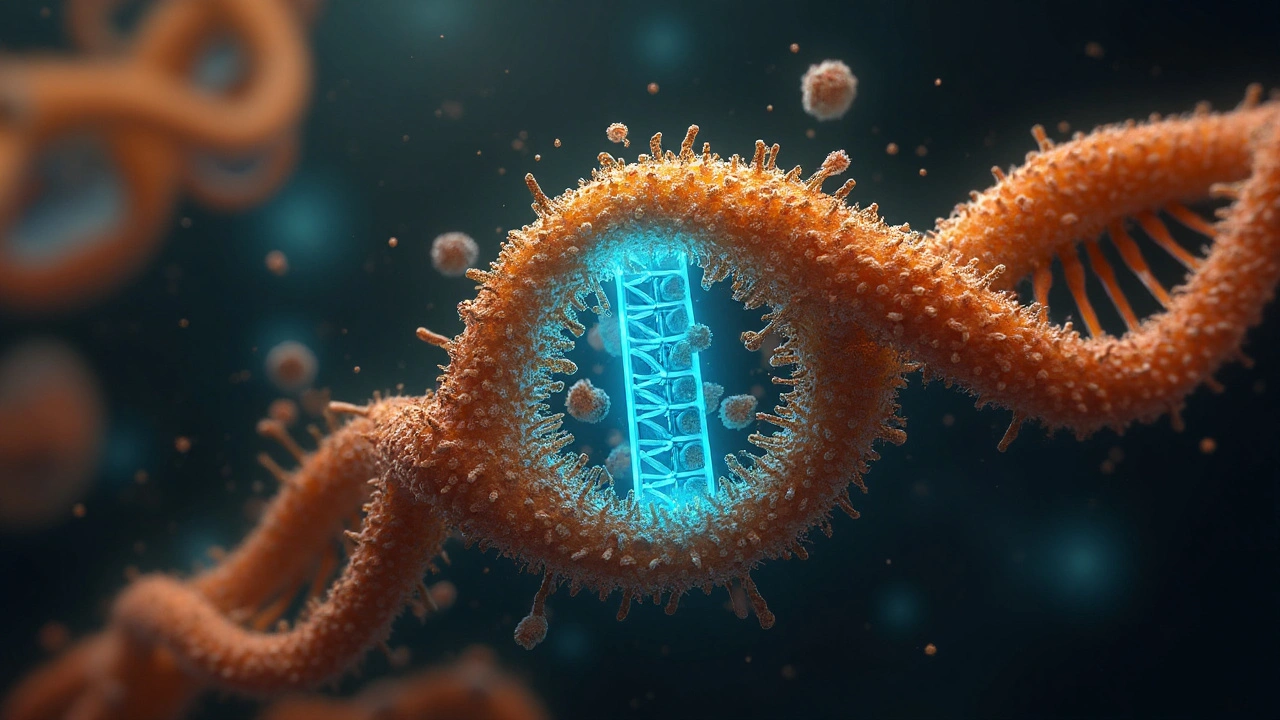
Understanding the Bacterial Ribosome
The bacterial ribosome consists of a 50S large subunit and a 30S small subunit. The 50S subunit houses the peptidyl‑transferase center (PTC), the catalytic heart where peptide bonds form. Unlike eukaryotic ribosomes, the bacterial PTC has distinct rRNA sequences that allow selective drug targeting.
When a ribosome starts translating mRNA, several initiation factors (IF1, IF2, IF3) help position the start codon. Linezolid’s action bypasses these factors by freezing the ribosome in a pre‑initiation state.
Linezolid’s Exact Molecular Hook
The drug slots into a pocket formed by nucleotides of the 23S rRNA in the PTC. This pocket lies adjacent to the A‑site (amino‑acyl‑tRNA entry site) and the P‑site (peptidyl‑tRNA site). By occupying this niche, linezolid blocks the formation of the first peptide bond, halting translation at the very start of protein synthesis.
Because the binding site is highly conserved across Gram‑positive bacteria, linezolid retains activity against a broad spectrum of strains, including those that produce altered penicillin‑binding proteins or thickened cell walls.
Comparing Linezolid with Its Peers
| Drug | Class | Spectrum (Gram‑positive) | Oral Bioavailability | Dosing Frequency | Resistance Risk |
|---|---|---|---|---|---|
| Linezolid | Oxazolidinone | MRSA, VRE, Streptococcus spp. | ≈90% | Every 12h | Low‑to‑moderate (mutations in 23S rRNA) |
| Tedizolid | Oxazolidinone (next‑gen) | Similar to linezolid, added activity against some linezolid‑resistant strains | ≈90% | Once daily | Very low (higher binding affinity) |
| Vancomycin | Glycopeptide | MRSA, CoNS, Enterococcus spp. | Negligible (IV only) | Every 12h (IV) | Increasing (VanA/VanB gene clusters) |
Clinical Implications of the Binding Mechanism
Because linezolid stops protein synthesis at an early step, bacteria cannot produce essential enzymes, toxins, or structural proteins. This rapid shut‑down translates to bacteriostatic activity in most strains, but at higher concentrations or in certain pathogens (e.g., Streptococcus pneumoniae) it can be bactericidal.
The early block also means linezolid is less affected by bacterial efflux pumps that often expel drugs from the cytoplasm. However, overuse can select for mutations in the 23S rRNA gene (G2576T, G2447U) that diminish binding.
Resistance: How Bacteria Fight Back
Three primary routes have emerged:
- Point mutations in domain V of the 23S rRNA, lowering affinity for the drug.
- Acquisition of the cfr gene, which methylates adenine 2503, sterically hindering linezolid binding.
- Up‑regulation of efflux pumps (e.g., OptrA), though this is less common.
Surveillance data from the CDC (2023) show cfr‑mediated resistance in ~1% of MRSA isolates, primarily in Europe and Asia. While still rare, the trend underscores the need for stewardship.
Pharmacokinetics Tied to Mechanism
Linezolid’s small size (337Da) and lipophilic ring system enable it to cross the blood‑brain barrier, making it useful for CNS infections caused by susceptible Gram‑positive organisms. Its half‑life (~5-7h) aligns with the twice‑daily dosing schedule, maintaining plasma concentrations above the MIC for the majority of the dosing interval.
Renal excretion accounts for ~30% of clearance; the rest is metabolized via oxidative pathways. This means dose adjustment is rarely needed in renal dysfunction, but caution is advised in patients with prolonged therapy due to possible mitochondrial toxicity (thrombocytopenia, neuropathy).
Linking Mechanism to Adverse Effects
Because linezolid also binds to mitochondrial ribosomes-structures that resemble bacterial 70S ribosomes-extended use can impair mitochondrial protein synthesis. The resulting side‑effects (hematologic abnormalities, peripheral neuropathy) typically appear after two weeks of therapy.
Monitoring complete blood counts weekly during long courses helps catch early signs of toxicity, allowing clinicians to switch to an alternative agent.
Future Directions: New Oxazolidinones and Combination Strategies
Tedizolid, mentioned earlier, adds a hydroxymethyl group that strengthens binding to the PTC, improving potency and reducing resistance emergence. Trials (2024) show comparable efficacy to linezolid with only once‑daily dosing and a better safety profile.
Researchers are also exploring synergistic combos-linezolid plus daptomycin or ceftaroline-to overcome high‑inoculum infections and biofilm‑associated diseases. Early phase‑II data indicate additive killing without increased toxicity.
Take‑Home Summary
- Linezolid is an oxazolidinone that blocks the first peptide bond formation by binding to the 23S rRNA in the 50S ribosomal subunit.
- The mechanism gives it broad activity against MRSA, VRE, and other Gram‑positive pathogens, with excellent oral bioavailability.
- Resistance is still uncommon but rising via 23S rRNA mutations, cfr methylation, and efflux pumps.
- Therapeutic monitoring is crucial for long courses due to mitochondrial side‑effects.
- Next‑generation agents like tedizolid and strategic drug combos are shaping the future of oxazolidinone therapy.
Frequently Asked Questions
How does linezolid differ from vancomycin?
Linezolid is an oxazolidinone that inhibits protein synthesis by binding to the 50S ribosomal subunit, while vancomycin is a glycopeptide that blocks cell‑wall synthesis. Linezolid can be given orally with >90% bioavailability, whereas vancomycin must be administered intravenously. The two drugs also have distinct resistance mechanisms: linezolid resistance arises mainly from 23S rRNA mutations or cfr methylation, while vancomycin resistance is driven by VanA/B gene clusters that alter cell‑wall precursors.
Can linezolid be used for pneumonia?
Yes. Because linezolid penetrates lung tissue and the alveolar lining fluid well, it’s effective for community‑acquired and hospital‑acquired pneumonia caused by MRSA or other susceptible Gram‑positive organisms. Clinical trials have shown cure rates comparable to vancomycin, with the added convenience of oral dosing for step‑down therapy.
What monitoring is needed during long‑term linezolid therapy?
Weekly complete blood counts are recommended to detect thrombocytopenia or anemia early. Liver function tests should also be checked if therapy exceeds 14days, as rare hepatotoxicity can occur. Patients should be asked about peripheral neuropathy symptoms (tingling, numbness), which may signal mitochondrial toxicity.
Is linezolid effective against Gram‑negative bacteria?
No. Linezolid’s spectrum is confined to Gram‑positive organisms. Its binding site is absent in Gram‑negative ribosomes, and the outer membrane of Gram‑negatives prevents adequate drug entry. For Gram‑negative infections, beta‑lactams, fluoroquinolones, or carbapenems are required.
How does tedizolid improve on linezolid’s mechanism?
Tedizolid binds the same 23S rRNA pocket but with higher affinity due to a modified side chain. This translates into lower MIC values, a once‑daily dosing regimen, and a reduced risk of resistance because the drug can overcome many cfr‑mediated modifications that blunt linezolid’s activity.
What are the main side‑effects of short‑course linezolid treatment?
For courses under two weeks, side‑effects are typically mild: nausea, diarrhea, and headache. Severe adverse events like thrombocytopenia or peripheral neuropathy become more common with prolonged exposure (>14days).
Josephine Bonaparte
September 23, 2025 AT 03:24Linezolid really blocks the bacterial ribosome, no joke.
Meghan Cardwell
October 5, 2025 AT 20:57From a mechanistic standpoint, linezolid engages the peptidyl transferase center of the 50S ribosomal subunit, effectively stalling peptide bond formation. This oxazolidinone class leverages a unique binding pocket that circumvents traditional macrolide resistance pathways. Pharmacokinetically, its oral bioavailability hovers around 100%, making it a versatile agent for both inpatient and outpatient regimens. Clinically, the drug's bacteriostatic profile against staphylococci and enterococci underscores its utility in multi‑drug‑resistant infections.
Manno Colburn
October 18, 2025 AT 14:30When you stare at the microscopic battlefield, it dawns on you that every molecule is a tiny philosopher, debating the meaning of existence with the ribosome. Linezolid, in its stubborn grace, slips into the 23S rRNA like a rogue poet, insisting that the age‑old dance of translation be paused. The bacteria, naïve as a child in a candy store, cannot discern the subtlety of this molecular intrusion, and thus their protein synthesis grinds to a hesitant halt. Yet, this pause is not merely a mechanical hiccup; it is a profound statement about the limits of cellular ambition. In the grand theater of antimicrobial warfare, linezolid does not shout; it whispers, "I am here, you cannot build". The cfr gene, that sly mutineer, methylates the adenine at position 2503, effectively rewiring the binding site, a genetic coup d’état that renders the drug impotent. This resistance mechanism, while rare, illustrates the adaptive resilience encoded in bacterial genomes, an evolutionary improvisation that keeps the arms race alive. Moreover, the drug’s inhibition of mitochondrial protein synthesis in human cells explains the hematologic side effects, a reminder that even our therapeutic heroes have shadows. The incidence of thrombocytopenia after prolonged therapy is not a random accident but a mechanistic echo of ribosomal cross‑talk. Some clinicians argue that therapeutic drug monitoring can mitigate these hazards, turning a blunt instrument into a precision scalpel. Others counter that the simplicity of a fixed dosing regimen outweighs the complexity of individualized stewardship. Ultimately, the story of linezolid is a mosaic of chemistry, genetics, and clinical judgment, each tile reflecting a different facet of its impact. As we continue to decipher its pharmacodynamics, we uncover layers that challenge our assumptions about what an antibiotic can achieve. In the end, whether we view linezolid as a line‑drawing tool or a brushstroke in the microbial canvas depends on the perspective we choose to adopt. The saga continues, and each new study adds a stanza to this ever‑evolving poem of antimicrobial strategy.
Namrata Thakur
October 31, 2025 AT 07:04Adding to the earlier point, the inhibition of initiation complex formation means that even low‑level exposure can suppress early‑phase bacterial growth. This early brake often translates into better clinical outcomes for pneumonia and skin‑structure infections. It's a straightforward but powerful advantage that many overlook.
Chloe Ingham
November 13, 2025 AT 00:37And if you think the cfr‑mediated methylation is the only trick up bacteria's sleeve, think again. There are whispers of ribosomal mutations that subtly reshape the binding pocket, turning linezolid into a phantom foe. Some even suggest hidden plasmids ferrying resistance across continents, a silent caravan that evades surveillance. The stakes are higher than a single gene; it's a network of clandestine exchanges that could undermine our last‑line defenses.
Mildred Farfán
November 25, 2025 AT 18:10While the scientific depth is impressive, let’s not forget the cultural context-patients in low‑resource settings often receive linezolid without proper monitoring, leading to unexpected toxicities. A dash of cultural humility in prescribing can go a long way.
Danielle Flemming
December 8, 2025 AT 11:44Exactly! It’s like giving someone a powerful tool without a user manual. Educating both clinicians and patients about the need for regular blood counts can prevent those nasty side‑effects while still harnessing linezolid’s potency.
Anna Österlund
December 21, 2025 AT 05:17Let’s cut to the chase-if you’re dealing with MRSA, linezolid is a solid bet, but don’t ignore the price tag. It can burn a hole in the budget, so weigh the cost‑benefit carefully.
Brian Lancaster-Mayzure
January 2, 2026 AT 22:50I hear you. From a mentor’s perspective, I’d advise a stepwise approach: start with susceptibility testing, then consider pharmacoeconomic factors before committing to a full course.
Erynn Rhode
January 15, 2026 AT 16:24In practice, the synergy between susceptibility data and therapeutic drug monitoring creates a robust safety net. By tailoring dosage to patient‑specific pharmacokinetics, we can minimize hematologic risks while preserving efficacy. This strategy aligns with stewardship principles, ensuring that linezolid remains a viable option for future generations. Moreover, regular CBC checks every week, especially after two weeks of therapy, catch early declines in platelet counts before they become clinically significant. For patients with renal impairment, dose adjustments are crucial, as accumulation can amplify toxicity. Integrating electronic health record alerts for these checkpoints further streamlines the process, reducing the burden on busy clinicians. Ultimately, a proactive monitoring plan transforms linezolid from a high‑risk drug into a controlled, predictable therapy.
Rhys Black
January 28, 2026 AT 09:57Frankly, the casual glorification of linezolid overlooks the moral responsibility we hold as prescribers. Elevating a drug to a ‘miracle’ status invites complacency, ignoring the nuanced interplay of resistance, side effects, and cost. A disciplined, ethical approach is imperative.
Abhishek A Mishra
February 10, 2026 AT 02:24Totally agree, and it’s also worth noting that the cfr gene’s spread isn’t just a lab curiosity-it’s popping up in community isolates, which means we all need to stay vigilant.