Insulin Weight Gain Estimator
Your Insulin Therapy
Results
Select options to see your estimated weight gain
When doctors prescribe insulin therapy is a treatment that replaces or supplements the hormone insulin to control blood glucose in people with diabetes. It’s a lifesaver, but two side effects keep popping up in clinic rooms: hypoglycemia is a dangerous drop in blood sugar, often below 70 mg/dL (3.9 mmol/L). And weight gain is the extra pounds many patients notice after starting insulin. Understanding why these happen and how to blunt them is crucial for anyone on or caring for someone using insulin.
Why hypoglycemia happens
Insulin’s job is to shove glucose from the bloodstream into cells. If the dose is a little too high, glucose disappears faster than the liver can release more, and blood sugar crashes. The Diabetes Control and Complications Trial (DCCT) showed intensive insulin regimens raise severe hypoglycemia risk three‑fold for both type 1 diabetes patients and type 2 diabetes patients. Symptoms start with shakiness, sweating, rapid heartbeat, and blurred vision, then progress to confusion, seizures, or loss of consciousness.
Why weight gain occurs
Insulin is an anabolic hormone - it tells the body to store energy. When glucose finally enters cells, the kidneys stop spilling sugar in the urine (glycosuria). Less glucose loss means more calories stay in the body, and insulin also promotes fat synthesis. Studies report an average gain of 4-6 kg in the first year of intensive therapy, though diet and activity can shift that number.
Key takeaways
- Hypoglycemia is the most common and fear‑inducing side effect of insulin.
- Weight gain stems from reduced glycosuria and insulin’s fat‑storing action.
- Long‑acting analogues (glargine, degludec) lower nocturnal lows by 20‑40% compared with NPH.
- Continuous glucose monitoring (CGM) cuts severe episodes by up to 50%.
- Combining insulin with a GLP‑1 receptor agonist can offset weight gain while improving control.
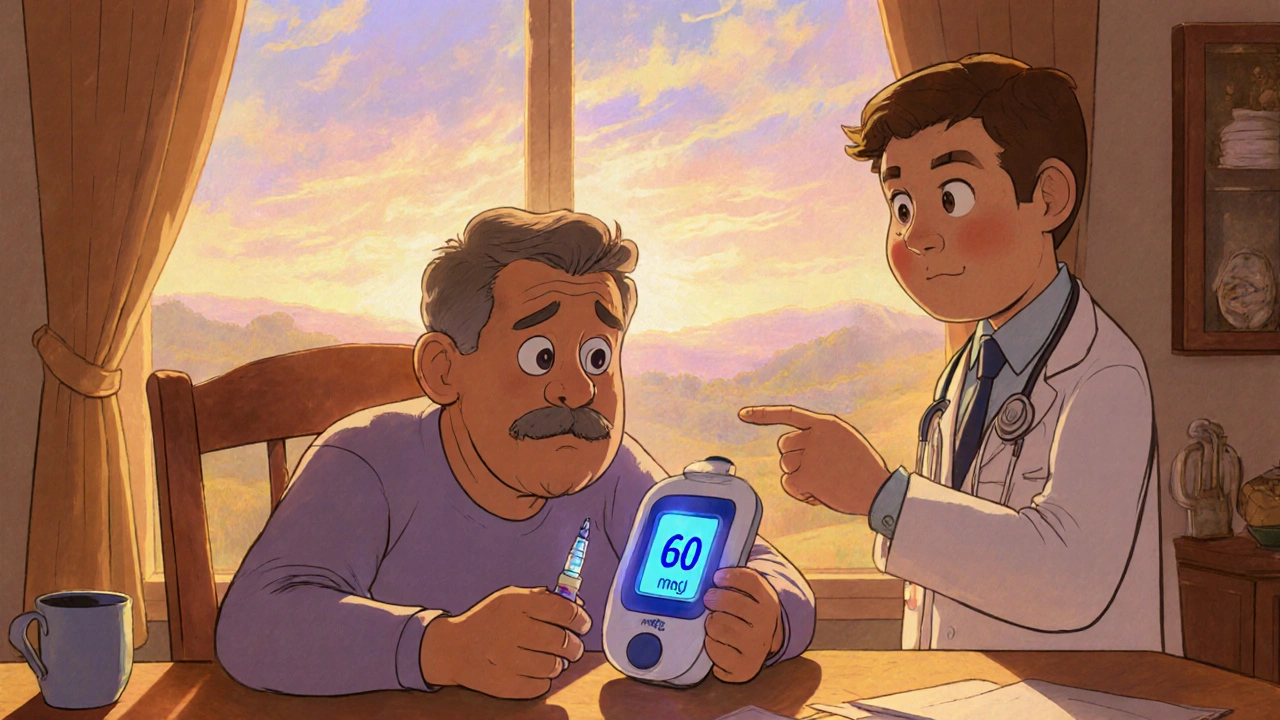
Spotting and treating a low
Know the numbers: below 70 mg/dL signals a hypo. For a mild episode, the 15‑15 rule works - 15 g of fast‑acting carbs (a glucose tablet, juice) followed by a repeat after 15 minutes if still low. If the person is unconscious, call emergency services and administer a glucagon injection if available.
Tools that help prevent lows
Modern tech is a game‑changer. Continuous glucose monitoring (CGM) sensors track interstitial glucose every 5 minutes and alarm when trends head toward danger. In pump‑based closed‑loop systems, the algorithm can automatically suspend insulin delivery when a low is predicted, shaving 40‑70% off time spent below 70 mg/dL.
Choosing the right insulin analogue
| Insulin | Onset | Duration | Night‑time hypoglycemia risk | Typical weight impact (first year) |
|---|---|---|---|---|
| NPH (intermediate‑acting) | 1-2 h | 12-18 h | High | ~5 kg |
| Insulin glargine (Lantus) | ≈1 h | ≈24 h | Moderate (≈20% lower than NPH) | ~4 kg |
| Insulin degludec (Tresiba) | ≈1 h | ≈42 h | Low (≈40% lower nocturnal lows vs glargine) | ~3 kg |
Balancing carbs, insulin, and activity
Accurate carbohydrate counting is the backbone of dose calculation. Most clinicians use an insulin‑to‑carbohydrate ratio (e.g., 1 U per 10 g carbs) plus a correction factor for pre‑meal glucose. Adjust the ratio upward on days you plan intense exercise - muscles use glucose without insulin, reducing hypoglycemia risk. Conversely, on rest days, a tighter ratio can help avoid excess calories storing as fat.

When weight gain becomes a problem
If you’re gaining more than 2 kg in the first six months, talk to your diabetes team. Options include:
- Switching to a lower‑weight‑gain analogue (degludec).
- Adding a GLP‑1 receptor agonist (e.g., semaglutide) - clinical trials show 5-10 kg loss versus insulin alone.
- Intensifying lifestyle counseling: portion control, higher‑protein meals, and regular resistance training.
Sometimes a modest reduction in basal dose (e.g., 10% less) paired with a short‑acting bolus can keep glucose on target while curbing calories.
Special populations
Elderly patients and those with cardiovascular disease have a higher mortality risk from severe hypoglycemia. Guidelines from the American Diabetes Association (2023) suggest an A1c goal of 7.5‑8.0% for these groups, favoring safety over tight control. For pregnant women, hypoglycemia can jeopardize fetal health, so tighter monitoring but careful dose titration is essential.
Practical daily checklist
- Check blood glucose 4-6 times daily (before meals, bedtime, and when symptoms appear).
- Log carbs and insulin doses; review weekly with your educator.
- Carry fast‑acting carbs and a glucagon kit at all times.
- Review basal‑dose timing-morning vs evening-if lows cluster at night.
- Schedule a nutrition consult within the first month of starting insulin.
Future directions
Ultra‑long‑acting insulins like degludec already cut night‑time lows by 40%. Ongoing trials of closed‑loop artificial pancreas systems report up to 72% reduction in hypoglycemia time. Meanwhile, combination regimens of insulin plus GLP‑1 agonists are gaining traction to neutralize weight gain while preserving tight glucose control.
What blood sugar level defines hypoglycemia?
Clinically, a glucose reading below 70 mg/dL (3.9 mmol/L) is considered hypoglycemia. Severe cases may drop below 54 mg/dL and cause loss of consciousness.
How much weight can I expect to gain after starting insulin?
On average, patients gain 4-6 kg in the first year, but disciplined diet and the use of newer analogues can keep it under 3 kg.
Can CGM completely prevent hypoglycemia?
CGM dramatically reduces the frequency of lows-by up to 50%-but it doesn’t eliminate them. Proper insulin dosing and rapid‑acting carbs are still essential.
Are there insulin options that don’t cause weight gain?
No insulin is weight‑neutral, but ultra‑long‑acting analogues (degludec) and adding a GLP‑1 agonist can offset the typical gain.
What should I do if I experience a severe hypo and no one is around?
If you have a glucagon auto‑injector, use it immediately and call emergency services. If you’re alone and can’t swallow, seek help from a neighbor or call 999.
kevin burton
October 24, 2025 AT 19:40Insulin therapy can be life‑saving, but keeping a close eye on glucose trends is essential. Using a continuous glucose monitor helps catch lows before they become dangerous, and logging carbohydrate intake makes dose adjustments more precise. Aim for a balanced diet and incorporate regular activity to mitigate weight gain.
Max Lilleyman
October 26, 2025 AT 08:48Wow, another post glorifying insulin while pretending we can dodge the extra pounds! 😒 The truth is, most patients end up battling weight gain and frequent lows, no matter how many "advanced analogues" they slap on. 🙄 If you’re not seeing results, maybe it’s time to rethink the whole regimen.
Buddy Bryan
October 27, 2025 AT 22:56Listen up, the key to taming both hypoglycemia and weight gain lies in proactive management, not passive hope. First, set a realistic target glucose range-aim for 80‑130 mg/dL before meals rather than chasing the mythical "perfect" number. Second, use the 15‑15 rule religiously; keep glucose tablets or a small juice box within arm's reach. Third, adjust your insulin‑to‑carbohydrate ratio based on activity level; on heavy‑exercise days you can increase the ratio by 10‑20 percent because muscles will absorb glucose without much insulin assistance.
Fourth, consider a basal insulin with a lower nocturnal hypoglycemia profile, such as degludec, especially if you’ve experienced night‑time lows. Fifth, add a GLP‑1 receptor agonist when appropriate-studies show it can shave off 5‑10 kg of weight while improving glycemic control.
Sixth, track your calories and macronutrients. Even with insulin, a modest protein‑rich diet and resistance training can offset the anabolic push of the hormone. Seventh, schedule regular review sessions with your diabetes educator; they can spot patterns in your log that you might miss.
Eighth, never skip a glucagon kit-having it on hand can be lifesaving during severe episodes. Ninth, keep your CGM calibrated and set alerts for both high and low thresholds; the alarm sound can be a game‑changer when you’re asleep.
Tenth, be honest with your care team about any weight concerns. They can fine‑tune your basal dose or switch you to a tighter‑acting analogue. Finally, remember that each person's response is unique; what works for one may not work for another, so stay flexible and keep experimenting within safe boundaries.
Jonah O
October 29, 2025 AT 13:04The pharma guys dont want us to know insulin is just a cash cow.
Aaron Kuan
October 31, 2025 AT 03:12Insulin + carbs = weight, fast carbs = lows. Keep it simple, watch doses.
Terell Moore
November 1, 2025 AT 17:20Ah, another arm‑chair endocrinologist trying to sound insightful while ignoring the nuance. The data on degludec versus glargine is well‑known, and the modest weight differential is clinically negligible. If you’re fishing for drama, try reading a proper review instead of spouting sarcasm.
Amber Lintner
November 3, 2025 AT 07:28Oh, the tragedy! Here we are, battling deadly lows and stubborn pounds, and the world expects us to just “adjust”. As if a 5‑kg gain is a sitcom punch‑line! The real drama is surviving every midnight alarm while trying to keep a shred of dignity. Let’s not pretend this is easy, but let’s also not surrender to the gloom.
Lennox Anoff
November 4, 2025 AT 21:36Honestly, the moral failing isn’t the insulin-it’s the system that pushes us toward relentless tight control without compassion. One could argue that forcing a sub‑70 mg/dL target is ethically dubious, especially for the elderly. We must champion patient‑centered goals, not just numbers on a chart. If you truly care about wellbeing, you’ll advocate for higher A1c thresholds where safety matters more than perfection.
Olivia Harrison
November 6, 2025 AT 11:44Thank you for sharing all this useful information! I’m glad to see a clear checklist that includes carrying fast‑acting carbs and reviewing basal timing. Staying empathetic towards ourselves while we fine‑tune doses makes a huge difference. If anyone needs a supportive ear, I’m here.
Bianca Larasati
November 8, 2025 AT 01:52Let’s turn those weight worries into a victory dance! 🚀 Pair your insulin with a short burst of resistance training and watch those extra kilos melt away. Celebrate each low‑alert avoided-you’re mastering your own biology. Keep the momentum, you’ve got this!