When you take more than one medication, your body doesn’t just process them separately. They interact-sometimes in ways that can be dangerous, sometimes in ways that make your treatment less effective. Understanding how these interactions work isn’t just for doctors and pharmacists. If you’re on multiple drugs-especially if you’re over 65 and taking five or more-you need to know the difference between pharmacokinetic and pharmacodynamic drug interactions. One changes how much drug gets to your system. The other changes how your body reacts to it. Mixing them up can lead to serious harm.
What Pharmacokinetic Interactions Do to Your Body
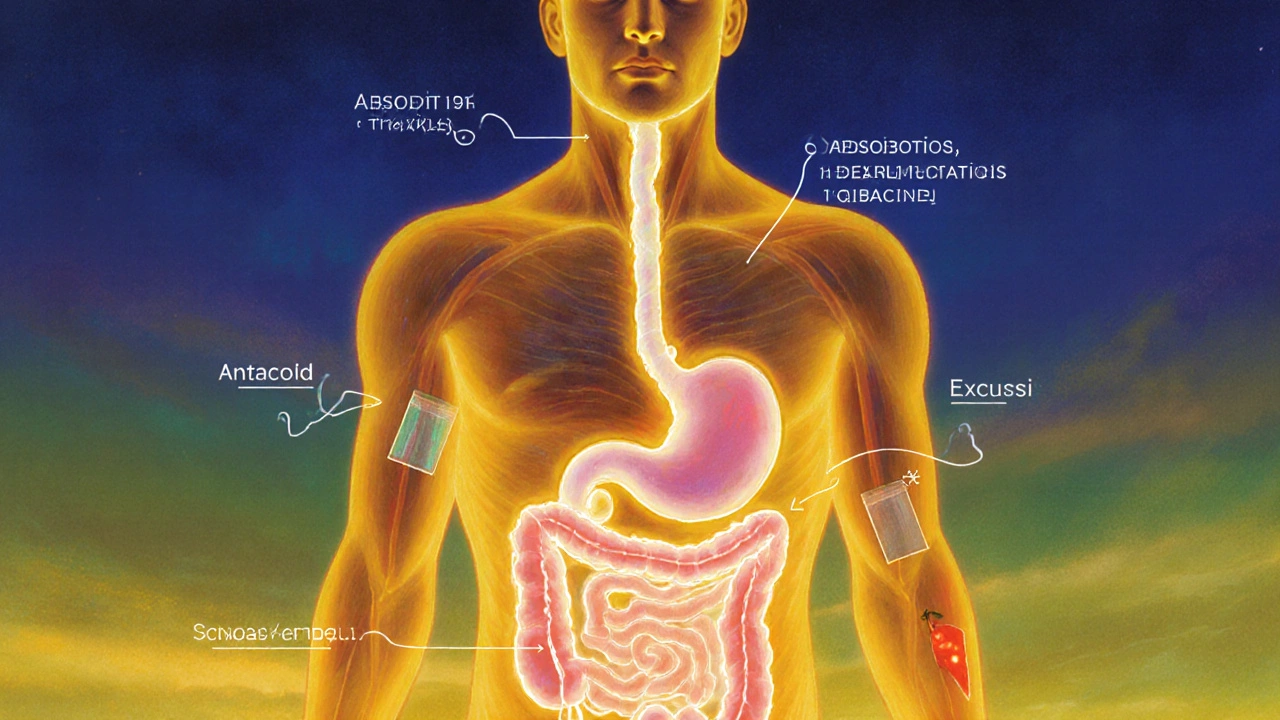
Pharmacokinetics, or PK, is what your body does to the drug. Think of it like a delivery system: how the drug gets in, moves around, gets broken down, and leaves. There are four key steps: absorption, distribution, metabolism, and excretion-often called ADME.A common PK interaction happens when one drug blocks another from being absorbed. Take antibiotics like ciprofloxacin. If you take it with an antacid, the magnesium or aluminum in the antacid binds to the antibiotic and stops it from being absorbed. Studies show this can reduce absorption by 75% to 90%. That means the antibiotic won’t work. You might think it’s not helping because your infection is stubborn, when really, your body never got enough of it.
Another big player is metabolism. Most drugs are broken down by enzymes in your liver, especially the CYP450 family. CYP3A4 handles about 50% of all prescription drugs. If you take clarithromycin (an antibiotic) with simvastatin (a cholesterol drug), clarithromycin shuts down CYP3A4. That means simvastatin can’t break down. Its levels in your blood can spike up to 10 times higher than normal. That’s not just a little extra-it can cause muscle damage, kidney failure, even death. The FDA recommends cutting simvastatin to 10mg or switching to another statin if you’re on clarithromycin.
Then there’s distribution. Some drugs, like warfarin, stick tightly to proteins in your blood. If another drug, like phenylbutazone, comes along and pushes warfarin off those proteins, suddenly you’ve got way more free warfarin floating around. That’s a 300% increase in active drug. You’re at risk of serious bleeding-even if your dose hasn’t changed.
Excretion matters too. Probenecid, used for gout, blocks the kidneys from flushing out penicillin. That keeps penicillin in your system longer, boosting its effect. But if you’re on a drug that needs to be cleared quickly, this could cause toxicity.
What Pharmacodynamic Interactions Do to Your Body
Pharmacodynamics, or PD, is what the drug does to your body. It’s not about concentration-it’s about effect. Two drugs can be at perfect levels in your blood, but if they both hit the same system, things can go wrong.There are three types of PD interactions: synergistic, additive, and antagonistic.
Synergistic means the combined effect is stronger than the sum of each drug alone. Take sildenafil (Viagra) and nitroglycerin. Sildenafil relaxes blood vessels. Nitroglycerin does too. Together, they can drop your blood pressure so hard you pass out-or worse. This combination is absolutely contraindicated. No exceptions.
Additive interactions are more common. Warfarin and aspirin both thin your blood. Together, they don’t multiply the effect-they just add up. That’s why your INR (a blood test for clotting) might creep up even if you haven’t changed your warfarin dose. Your doctor needs to watch that closely.
Antagonistic is when one drug cancels out another. Naloxone reverses opioid overdoses by kicking opioids off their receptors. Beta-blockers and beta-agonists do the same thing in the lungs and heart. If you’re on a beta-blocker for high blood pressure and you use an albuterol inhaler for asthma, the albuterol might not work as well. That’s not always obvious-until you’re wheezing and the inhaler isn’t helping.
PD interactions are especially tricky in the brain. Antidepressants, antipsychotics, and opioids often interact this way. Mixing SSRIs with MAO inhibitors can cause serotonin syndrome-a life-threatening surge in serotonin that leads to fever, seizures, and heart rhythm problems. That’s why doctors ask you to wait weeks between switching these drugs.

Why the Difference Matters for Your Safety
The biggest mistake people make is thinking all drug interactions are the same. They’re not. PK interactions can often be managed. PD interactions often need to be avoided entirely.If it’s a PK interaction-say, your blood thinner is being affected by an antibiotic-you might be able to adjust the dose, delay the antibiotic, or switch to a different one. Therapeutic drug monitoring (TDM) can help. Blood tests can show you exactly how much drug is in your system. That’s why people on warfarin, digoxin, or phenytoin get regular blood draws.
But with PD interactions, adjusting the dose doesn’t help. If two drugs are competing for the same receptor, lowering one won’t fix the clash. The only safe move is to stop one of them. That’s why you can’t take NSAIDs like ibuprofen with ACE inhibitors for blood pressure. The NSAID blocks the kidney’s ability to respond to the ACE inhibitor. Your blood pressure stays high, even though you’re taking your pills. You won’t know until your next checkup.
According to the Specialist Pharmacy Service in the UK, 68% of dangerous interactions with narrow-therapeutic-index drugs (like warfarin or lithium) are PK-based. But for drugs that affect the heart or brain, PD interactions are the main concern. Over 78% of CNS drug interactions are pharmacodynamic. That’s why your pharmacist asks if you’re taking anything for anxiety, sleep, or pain-because those are the most likely to cause silent, deadly clashes.
How Clinicians Spot These Interactions
Doctors and pharmacists don’t guess. They use tools. Electronic health records now flag interactions based on databases like the Flockhart Table, which lists over 2,000 known drug interactions. Epic’s 2023 system alone warns about 1,247 high-risk PK interactions and 983 high-risk PD interactions.But even the best system misses things. That’s why pharmacist-led medication reviews work. A 2022 survey by the American College of Clinical Pharmacy found that when pharmacists actively manage drug regimens, adverse events from interactions drop by 42%. That’s not magic-it’s knowing what to look for.
For PK interactions, they watch timing. CYP3A4 inhibitors like clarithromycin take 3 to 5 days to reach full effect. So if you start feeling muscle pain a week after starting an antibiotic with your statin, that’s a red flag. For PD interactions, they watch symptoms. If your breathing slows after adding a new sleep aid, or your blood pressure suddenly spikes after starting a new painkiller, it’s not coincidence-it’s interaction.
Real-world data from the FDA’s Sentinel Initiative found new PD risks, like SGLT2 inhibitors (used for diabetes) combined with loop diuretics. Together, they double the risk of dehydration. That wasn’t known until thousands of patient records were analyzed. That’s how medicine is evolving.

What You Can Do Right Now
You don’t need to memorize enzyme names or receptor pathways. But you can protect yourself.- Keep a full list of every medication you take-prescription, over-the-counter, vitamins, supplements. Include doses and why you take them.
- Ask your pharmacist: “Could any of these interact?” Don’t wait for them to bring it up. Bring your list every time you refill.
- If you start a new drug and feel unusual symptoms within hours or days, note them. Did your dizziness start after adding a new painkiller? Did your swelling get worse after a new blood pressure pill? Tell your doctor immediately.
- Don’t assume natural products are safe. St. John’s wort can knock down levels of antidepressants, birth control, and heart meds by up to 60% through enzyme induction. It’s a PK interaction, and it’s dangerous.
- If you’re on a drug with a narrow therapeutic index-warfarin, digoxin, lithium, phenytoin, or cyclosporine-stick to the same brand and pharmacy. Small changes in formulation can trigger PK shifts.
Most importantly: if your doctor says, “This combination is risky,” don’t argue. They’re not being cautious-they’re being accurate. The science is clear. PK interactions can be managed. PD interactions often can’t. And when they hit, they hit fast.
What’s Changing in Drug Interaction Science
The field is moving fast. The FDA now requires testing against 11 CYP enzymes and 8 transporters-up from just 7 in 2017. Pharmacogenomics is becoming part of the equation. If you’re a poor metabolizer of CYP2D6, even a normal dose of codeine might turn into a dangerous amount of morphine. That’s a PK interaction shaped by your genes.AI models are getting better at predicting PD interactions. A 2023 study in Nature Medicine showed an AI system predicting dangerous combinations with 89% accuracy-better than traditional methods. That means in the future, your electronic prescription might warn you not just about known risks, but about hidden ones based on patterns from millions of patients.
But the biggest win? The WHO estimates that better understanding of PK and PD interactions could prevent 1.3 million adverse drug events worldwide by 2030. That’s not just numbers-it’s lives saved. And it starts with knowing the difference between what your body does to the drug, and what the drug does to your body.
What’s the main difference between pharmacokinetic and pharmacodynamic interactions?
Pharmacokinetic (PK) interactions change how much of the drug reaches your bloodstream-through absorption, metabolism, or excretion. Pharmacodynamic (PD) interactions change how your body responds to the drug, even if the level stays the same. PK is about concentration; PD is about effect.
Can pharmacokinetic interactions be fixed with dose changes?
Yes, often they can. If one drug slows the metabolism of another, lowering the dose of the affected drug can prevent toxicity. For example, reducing simvastatin to 10mg when taking clarithromycin avoids muscle damage. Therapeutic drug monitoring helps guide these adjustments.
Why are pharmacodynamic interactions harder to predict?
Because they depend on how drugs affect your body’s systems-not just their levels. Two drugs can be at safe concentrations but still cause dangerous effects if they both lower blood pressure, depress breathing, or overstimulate serotonin. These effects aren’t always obvious until symptoms appear.
Which drugs are most likely to cause dangerous interactions?
Drugs with a narrow therapeutic index-like warfarin, digoxin, lithium, and phenytoin-are most vulnerable to PK interactions. For PD interactions, central nervous system drugs (antidepressants, opioids, benzodiazepines), anticoagulants, and cardiovascular drugs (like ACE inhibitors and NSAIDs) carry the highest risk.
Should I stop taking my meds if I’m worried about interactions?
Never stop a prescribed medication without talking to your doctor or pharmacist. Many interactions can be managed safely with adjustments. But if you notice new symptoms-dizziness, bleeding, confusion, swelling, or breathing changes-contact your provider right away. Don’t wait.
Do supplements and herbal products cause drug interactions?
Yes, and they’re often overlooked. St. John’s wort can reduce levels of birth control, antidepressants, and heart meds by inducing liver enzymes. Garlic and ginkgo can increase bleeding risk with warfarin. Even high-dose vitamin E can thin your blood. Always tell your pharmacist about everything you take.
How often should I review my medications with a pharmacist?
At least once a year, or anytime you start or stop a medication, change doses, or see a new doctor. If you’re over 65 and taking five or more drugs, quarterly reviews are recommended. Pharmacists are trained to catch interactions that doctors might miss in a busy appointment.
Joseph Peel
November 17, 2025 AT 14:58Pharmacokinetic interactions are the silent saboteurs of medication efficacy. I’ve seen patients on warfarin whose INR spiked after starting omeprazole-no one told them proton pump inhibitors inhibit CYP2C9. The fix? Switch to pantoprazole. Simple. But patients don’t know this unless someone explains it. The ADME framework isn’t just for pharmacists-it’s essential life knowledge for anyone on more than three meds.
And don’t get me started on grapefruit juice. It’s not a myth-it’s a CYP3A4 grenade. One glass can turn a safe statin dose into a rhabdomyolysis risk. If you’re on simvastatin or atorvastatin, avoid it entirely. No exceptions.
Kelsey Robertson
November 18, 2025 AT 07:32Let’s be honest: this whole PK/PD distinction is just academic theater… unless you’re the one bleeding out because someone didn’t realize that fluoxetine and tramadol together can trigger serotonin syndrome-*after* you’ve been on both for months.
And yet, people still think ‘natural’ means ‘safe.’ St. John’s wort? It’s a CYP inducer with the subtlety of a jackhammer. It doesn’t just ‘interact’-it obliterates therapeutic levels of birth control, antidepressants, even transplant meds. And no, your ‘herbalist’ isn’t a doctor. They’re a liability with a website.
Also-why do we still let people self-prescribe NSAIDs? Ibuprofen + ACE inhibitor = renal failure waiting to happen. But sure, take two Advil because your back ‘hurts.’
Elia DOnald Maluleke
November 19, 2025 AT 12:50It is not merely a matter of biochemical pathways; it is a question of human vulnerability in the face of pharmaceutical complexity. We live in an age where the body is treated as a machine-yet we forget that it is a symphony of interdependent systems, each note amplified or silenced by the next.
When a drug alters the metabolism of another, it is not a technical glitch-it is an interruption of the body’s sacred rhythm. And when two drugs converge upon the same receptor, it is not a pharmacological coincidence-it is a collision of intentions.
Consider the elderly: they are not merely ‘polypharmacy patients.’ They are the living archives of medical progress, each pill a chapter in a story written by specialists who never spoke to one another. And yet, we expect them to remember which pill does what-when even the clinicians struggle.
This is not science. This is survival.
satya pradeep
November 19, 2025 AT 22:51Bro, this is why you gotta keep a list. I had my uncle on warfarin and he started taking turmeric ‘for inflammation.’ Didn’t tell anyone. Ended up in ER with a GI bleed. Turns out turmeric is a mild anticoagulant-so now he’s on DOACs and no more ‘natural remedies’ without asking first.
Also-CYP3A4 is the OG drug killer. Clarithromycin + statin? Big no. Even OTC stuff like dextromethorphan can mess with SSRIs. And yeah, St. John’s wort? It’s basically a chemical grenade in a tea bag.
Pharmacists are your real MVPs. Talk to them. Not just your doctor. They see the whole picture. And if you’re over 65? Quarterly med review. No excuses.
Prem Hungry
November 20, 2025 AT 15:08Thank you for writing this with such clarity. As someone who helps elderly patients navigate their medication regimens, I can tell you-this is the single most overlooked issue in primary care.
Many seniors are on 7–10 medications. They take them at different times. Some are from different doctors. No one connects the dots. And when they feel dizzy or swollen or confused, they blame aging-not drug interactions.
I always tell them: ‘Your body is not broken. It’s just overloaded.’ A simple med review with a pharmacist can prevent hospitalization. I’ve seen it happen. One woman stopped her NSAID, switched her blood pressure med, and her kidney numbers normalized in two weeks.
Don’t wait for a crisis. Bring your list. Ask the questions. You are your own best advocate.
Jessica Healey
November 22, 2025 AT 03:52I just started a new antidepressant and now I can’t sleep, my hands shake, and I feel like I’m going to pass out. I thought it was ‘adjustment’ but now I’m terrified. Is this serotonin syndrome? Am I going to die? I didn’t know mixing it with my melatonin could do this. I feel so stupid.
Levi Hobbs
November 23, 2025 AT 18:53Thank you for sharing that, Jessica. You’re not stupid-this is exactly why we need better patient education. Serotonin syndrome can start subtly: tremors, sweating, agitation. Melatonin isn’t the culprit-it’s likely the combo of your SSRI and a supplement like 5-HTP or tryptophan. But you’re right to be alarmed. Call your prescriber today. Don’t wait. And please, keep that med list updated.
Also-this post is spot-on. PK is about concentration; PD is about effect. And PD is the silent killer because it doesn’t show up on labs. It shows up in your pulse, your breathing, your confusion.
henry mariono
November 24, 2025 AT 12:22I’m on warfarin and take a daily omega-3. My INR’s been stable for years. Should I stop it?