Quick Takeaways
- Baclofen is a GABA‑B receptor agonist traditionally used as a muscle relaxant.
- Emerging data suggest it can reduce involuntary movements in some people with tardive dyskinesia (TD).
- Typical starting dose is 5 mg three times daily, titrated up to 20‑30 mg three times daily based on response and tolerance.
- Common side effects include drowsiness, weakness, and low blood pressure; severe reactions are rare.
- Compared with FDA‑approved TD drugs like valbenazine, baclofen is cheaper but has less robust evidence.
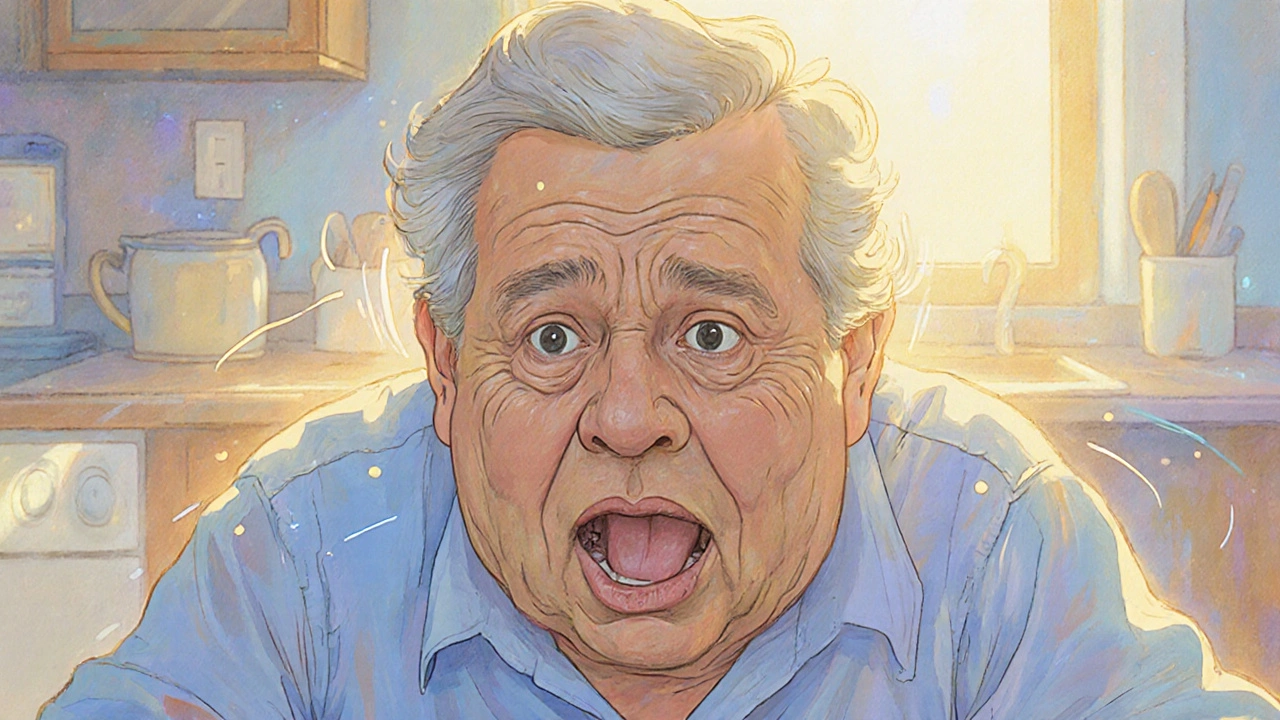
What Is Tardive Dyskinesia?
Imagine a person trying to speak, eat, or smile, only to have their face twitch uncontrollably. That’s the reality of Tardive Dyskinesia is a chronic movement disorder characterized by repetitive, involuntary muscle contractions, most often affecting the facial muscles, tongue, and limbs. It usually develops after months or years of exposure to dopamine‑blocking medications, especially antipsychotics.
The condition can be socially disabling and is often mistaken for anxiety or psychosis side‑effects. Once established, the movements tend to persist even after the offending drug is stopped, which is why clinicians look for treatments that target the underlying neurochemistry.
How baclofen Works: The Mechanism Behind the Muscle Relaxant
Baclofen is a selective GABA‑B receptor agonist that dampens excitatory signals in the spinal cord and brain. By activating these inhibitory receptors, baclofen reduces muscle tone, which is why it’s prescribed for spasticity in conditions like multiple sclerosis or spinal cord injury.
In the context of TD, the hypothesis is that enhancing GABA‑B activity can modulate the overactive dopaminergic pathways that drive the abnormal movements. While it doesn’t block dopamine directly, it creates a counter‑balance that may calm the motor circuits.
Scientific Evidence: Does Baclofen Really Help TD?
A handful of small‑scale studies and case reports have explored baclofen for TD. One 2022 open‑label trial involving 30 patients reported a mean 30 % reduction in the Abnormal Involuntary Movement Scale (AIMS) score after 12 weeks of titrated baclofen (up to 20 mg three times daily). Another case series from 2021 highlighted two patients who experienced near‑complete remission of facial dyskinesia after adding baclofen to their regimen.
However, larger randomized controlled trials are still missing, and the existing data are limited by short follow‑up periods and lack of placebo groups. Experts therefore label baclofen as an “off‑label adjunct” rather than a first‑line therapy.
Dosage and Administration: Getting the Numbers Right
Because baclofen can cause sedation and weakness, clinicians start low and go slow. A typical titration schedule looks like this:
- Day 1‑3: 5 mg orally three times daily.
- Day 4‑7: Increase to 10 mg three times daily if tolerated.
- Week 2 onward: Continue to raise by 5 mg per dose every 3‑5 days until the desired effect or side‑effects limit further increase.
Most patients find a therapeutic window between 20 mg and 30 mg three times daily. Doses above 80 mg total per day are rarely needed for TD and increase the risk of hypotension and respiratory depression.
For patients with renal impairment, dose adjustments are recommended because baclofen is primarily excreted unchanged in the urine.
Benefits and Potential Risks
When baclofen works, the benefits are clear: reduced choreiform movements, improved facial expression, and better quality of life. The drug’s oral formulation makes it easy to incorporate into existing medication schedules.
On the downside, the most common side effects are:
- Drowsiness or fatigue.
- Muscle weakness, which can affect gait.
- Dizziness or light‑headedness, especially when standing quickly.
- Dry mouth and constipation.
Rare but serious reactions include seizures (usually after abrupt discontinuation) and severe hypotension. Tapering the medication slowly-cutting the dose by 10‑20 % every few days-is essential to avoid withdrawal.
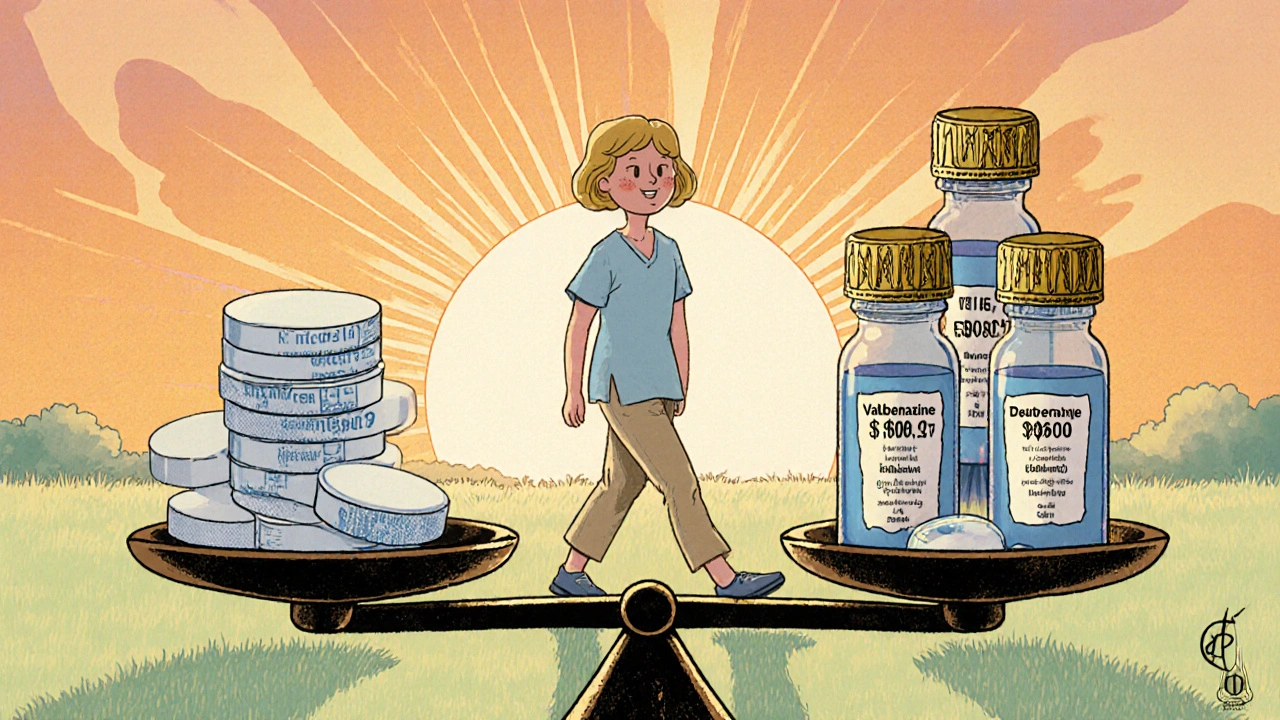
How Baclofen Stacks Up Against Other TD Treatments
Several FDA‑approved drugs target TD more directly, primarily by reducing dopamine release. Below is a quick side‑by‑side look at the most common options.
| Drug | Mechanism | Typical Dose | Evidence Strength | Cost (USD/ month) |
|---|---|---|---|---|
| Baclofen | GABA‑B agonist (muscle relaxant) | 5‑30 mg TID | Low‑to‑moderate (small trials) | ~$15 |
| Valbenazine | VMAT2 inhibitor (reduces dopamine release) | 40‑80 mg daily | High (Phase III RCTs) | ~$2,800 |
| Deutetrabenazine | VMAT2 inhibitor, deuterated | 12‑24 mg TID | High (Phase III RCTs) | ~$3,200 |
| Clonazepam | Benzodiazepine (GABA‑A enhancer) | 0.5‑2 mg BID‑TID | Moderate (open‑label) | ~$30 |
Key takeaways from the table: baclofen is far cheaper but lacks the robust trial data that VMAT2 inhibitors have. If cost is a major barrier, baclofen can be a reasonable trial, especially when combined with other strategies like speech therapy or behavioral interventions.
Practical Tips for Patients and Clinicians
Here’s a short checklist you can use the next time you discuss baclofen for TD:
- Assess baseline AIMS score. Document severity before starting.
- Start low (5 mg TID) and titrate slowly; watch for dizziness.
- Schedule regular follow‑ups every 2‑4 weeks during titration.
- Consider adding a low‑dose benzodiazepine if sedation becomes an issue.
- Educate the patient about the need for a gradual taper if stopping.
- Monitor renal function, especially in older adults.
From a clinician’s perspective, it’s also wise to review the patient’s full medication list. Certain drugs-like other CNS depressants-can amplify baclofen’s side effects.
Frequently Asked Questions
Can baclofen cure tardive dyskinesia?
No. Baclofen can lessen the severity of involuntary movements for some people, but it does not eradicate the underlying disorder. It’s best viewed as a symptomatic adjunct.
Is baclofen approved by the FDA for TD?
No. Baclofen is FDA‑approved for spasticity, not for tardive dyskinesia. Its use in TD is off‑label.
How long does it take to see improvement?
Most clinicians report noticeable changes within 4‑6 weeks of reaching a stable dose, though full benefits may take up to 12 weeks.
What should I do if I feel overly sleepy?
Try lowering the dose by one step and see if the drowsiness improves. If it persists, discuss switching to an alternative TD medication with your prescriber.
Can baclofen be combined with valbenazine?
There’s limited data on the combination, but some clinicians use low‑dose baclofen alongside a VMAT2 inhibitor when the response to a single agent is inadequate. Close monitoring for additive sedation is essential.
Bottom Line
If you’re battling TD and standard therapies are out of reach, a trial of baclofen could be worth considering. Its low cost and oral form make it attractive, but remember the evidence is still modest. Talk with your neurologist or psychiatrist, start low, watch for side effects, and keep a symptom diary to gauge real progress.
Rhea Lesandra
October 26, 2025 AT 13:32If you’re weighing baclofen as a supplement for tardive dyskinesia, start by mapping your baseline AIMS score and discuss the titration plan with your clinician. The drug’s low cost can be a real advantage for many patients who can’t afford newer VMAT2 inhibitors. Remember that the typical starting point is 5 mg three times daily and you should move up slowly while watching for drowsiness or weakness. Because it works on GABA‑B receptors, it may help balance the over‑active dopaminergic pathways that drive involuntary movements. Keep a symptom diary; objective data will guide whether the medication is making a meaningful difference for you.
Dave Sykes
October 28, 2025 AT 08:44From a coaching perspective, the key is consistency and monitoring. Stick to the low‑and‑slow titration schedule and give the body at least two weeks at each dose before deciding if you need more. If you notice persistent sedation, cut back a step rather than abandoning the trial entirely. Pair the medication with a structured physical therapy routine to maximize functional gains. This disciplined approach often separates a successful adjunct from a wasted effort.
Erin Leach
October 30, 2025 AT 03:56I hear you on the frustration of dealing with TD and the search for affordable options. Baclofen can be a gentle start, especially if you already have kidney concerns where dose adjustments matter. Staying casual, just remember to drink plenty of water and keep an eye on blood pressure when you first raise the dose. It’s okay to feel a bit off at first; many people report a week of mild fatigue before steadier improvement appears. Keep an open line with your prescriber-you’re not alone in this.
Erik Redli
October 31, 2025 AT 23:08While Dave’s advice sounds nice it forgets the hard truth: baclofen’s evidence is flimsy and the side‑effect profile can knock you out of your day. You’re basically swapping one set of problems for another, and the aggressive push to “stick with it” can be dangerous if you’re not monitored hourly. The drug’s sedation can mask worsening dyskinesia, leading you to think it works when it’s just dulling your senses. I’d challenge anyone to put baclofen through a proper double‑blind trial before preaching its virtues.
Paul Luxford
November 2, 2025 AT 18:20I appreciate the range of opinions shared here and want to add a balanced note. The cost benefit of baclofen is real, yet the data gap means we should proceed with caution. Respectful monitoring and clear boundaries on dose escalation protect patients from unnecessary risk. An open‑minded dialogue between prescriber and patient helps tailor therapy to individual tolerance.
Nic Floyd
November 4, 2025 AT 13:32From a pharmacodynamic standpoint baclofen acts as a selective GABAB agonist modulating presynaptic inhibition of excitatory neurotransmission its efficacy in spasticity is well documented the extrapolation to tardive dyskinesia hinges on the hypothesized dopaminergic‑GABAergic interplay however the paucity of phase III data limits definitive conclusions the dose‑response curve appears sigmoidal with a therapeutic window between 20‑30 mg TID beyond which adverse events such as hypotension and central sedation rise precipitously clinicians should employ a titration schema incremental 5 mg increments every 3‑5 days while tracking AIMS scores in a longitudinal fashion the renal clearance pathway necessitates dose adjustment in CKD stage 3+ patients to avoid accumulation the cost differential relative to valbenazine is substantial ~$15 versus $2800 per month making baclofen an attractive off‑label adjunct for resource‑constrained settings however vigilance for withdrawal seizures upon abrupt cessation is paramount ensure a tapering protocol of 10‑20 % reduction every few days 😊
Johnae Council
November 6, 2025 AT 08:44Alright, let’s cut the fluff. Baclofen is basically a cheap high‑risk gamble. People love to hype it because it’s cheap, but the side‑effects-drowsiness, weakness, even seizures on stop-are real and can wreck lives. The data? A handful of tiny open‑label studies that don’t even shake the confidence interval. If you want a medication that actually works, you might as well go straight to the FDA‑approved VMAT2 inhibitors and save yourself the headache.
Manoj Kumar
November 8, 2025 AT 03:56Isn’t it charming how we all pretend a cheap muscle relaxer can “solve” a complex neuro‑psychiatric condition? Sarcastically, sure, let’s all hop on the baclofen bandwagon while the pharma giants sit back watching us scramble for the next cheap fix. Optimistically, maybe a modest reduction in tremor is better than none, but let’s not kid ourselves into thinking we’ve cured tardive dyskinesia with a GABA‑B kiss. The philosophy here is simple: short‑term comfort isn’t a substitute for robust, evidence‑based therapy.
Hershel Lilly
November 9, 2025 AT 23:08I echo Nic’s technical points about dosage and renal adjustment but would add that a multidisciplinary approach-neurology, physiotherapy, and occupational therapy-often yields better functional outcomes than medication alone. Monitoring AIMS scores quarterly provides objective data to guide incremental dose changes.
Carla Smalls
November 11, 2025 AT 18:20Take it slow and listen to your body.