Generic vs Brand Drugs: What You Really Need to Know
When you pick up a prescription, you might see two options: a generic drug, a medication that contains the same active ingredient as a brand-name drug but is sold under its chemical name after the patent expires. Also known as generic medication, it works the same way, costs far less, and is held to the same FDA standards. The brand name drug, the original version developed by a pharmaceutical company and protected by patents. Also known as innovator drug, it carries the name you see advertised on TV and often costs 8 to 10 times more. Despite the price gap, both contain the same active ingredient, the component that actually treats your condition. Also known as therapeutic ingredient, it’s the reason your blood pressure drops, your infection clears, or your pain fades. The difference isn’t in what works—it’s in what’s hidden.
Here’s the catch: inactive ingredients—fillers, dyes, coatings, and preservatives—can vary between generic and brand versions. These don’t treat your condition, but they can affect how fast the drug dissolves, how it’s absorbed, or even trigger allergies in rare cases. That’s why some people notice a difference when switching, especially with drugs like thyroid meds or seizure controls where tiny changes matter. But for most people, switching to generic causes no issue at all. The FDA requires generics to be bioequivalent: they must deliver the same amount of active ingredient into your bloodstream at the same rate as the brand. Real-world data shows 90% of prescriptions in the U.S. are generic, and they save Americans over $300 billion every year. That’s not marketing—it’s math.
Still, not every brand has a generic. Some drugs are too complex to copy—think inhalers, biologics, or injectables with tricky delivery systems. Others stay expensive because companies use legal tricks to delay generics, like making minor changes to the formula just before the patent expires (called product hopping) or paying rivals to stay off the market (pay-for-delay). These tactics aren’t illegal everywhere, but they’re why your insulin or asthma inhaler still costs hundreds even after decades on the market. If you’re paying full price for a drug that should have a cheaper version, ask your pharmacist: is there a generic? Is there a therapeutic alternative? And most importantly—why aren’t you using it?
What follows are real stories, real numbers, and real advice from people who’ve been there: from the $5 generic that replaced a $400 brand, to the rare case where switching caused side effects, to how to spot when a generic might not be right for you. You’ll find breakdowns of drug savings, explanations of FDA approval timelines, and even how social media is changing how patients talk about generics. This isn’t theory. It’s what works, what doesn’t, and what you need to know before your next refill.
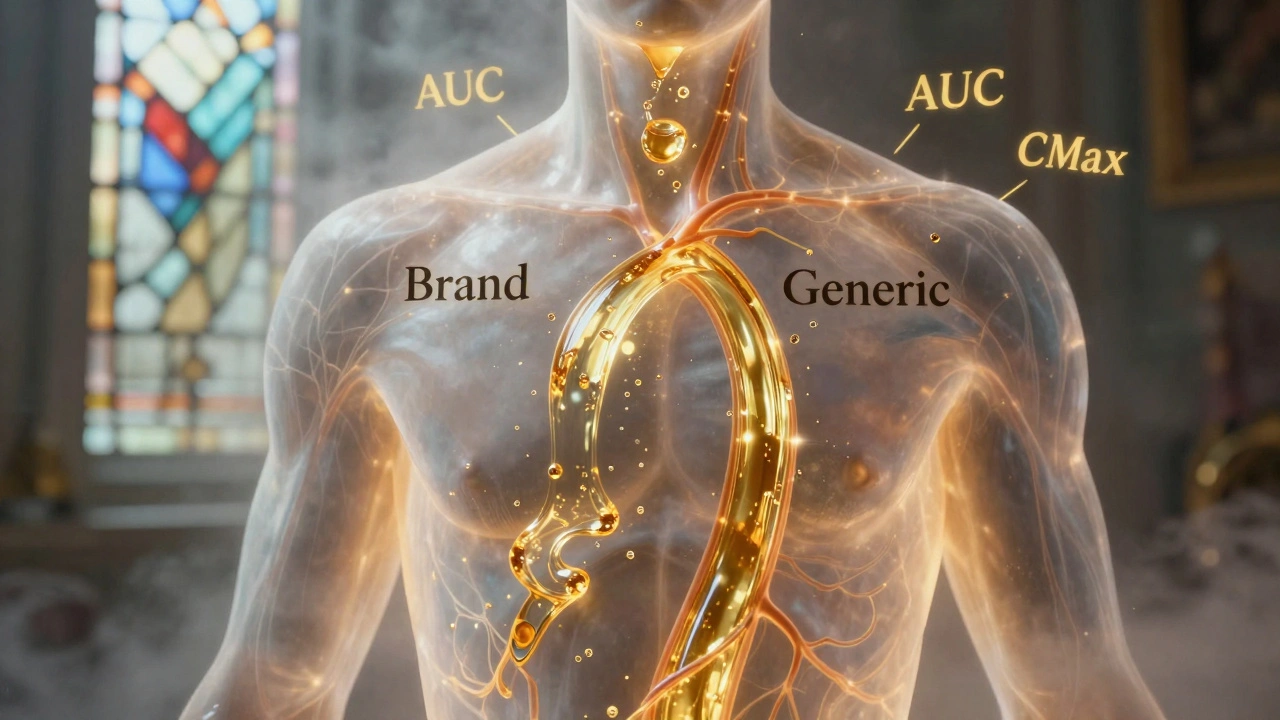
Generic Absorption Rates: How They Must Match Brand Drugs to Be Safe and Effective
Generic drugs must match brand-name absorption rates within strict 80-125% limits to be approved. Science shows they’re nearly identical in effectiveness - with only 3-5% average differences. Learn how bioequivalence works and why generics are safe.