Pharmacokinetic Interactions: How Drugs Affect Each Other in Your Body
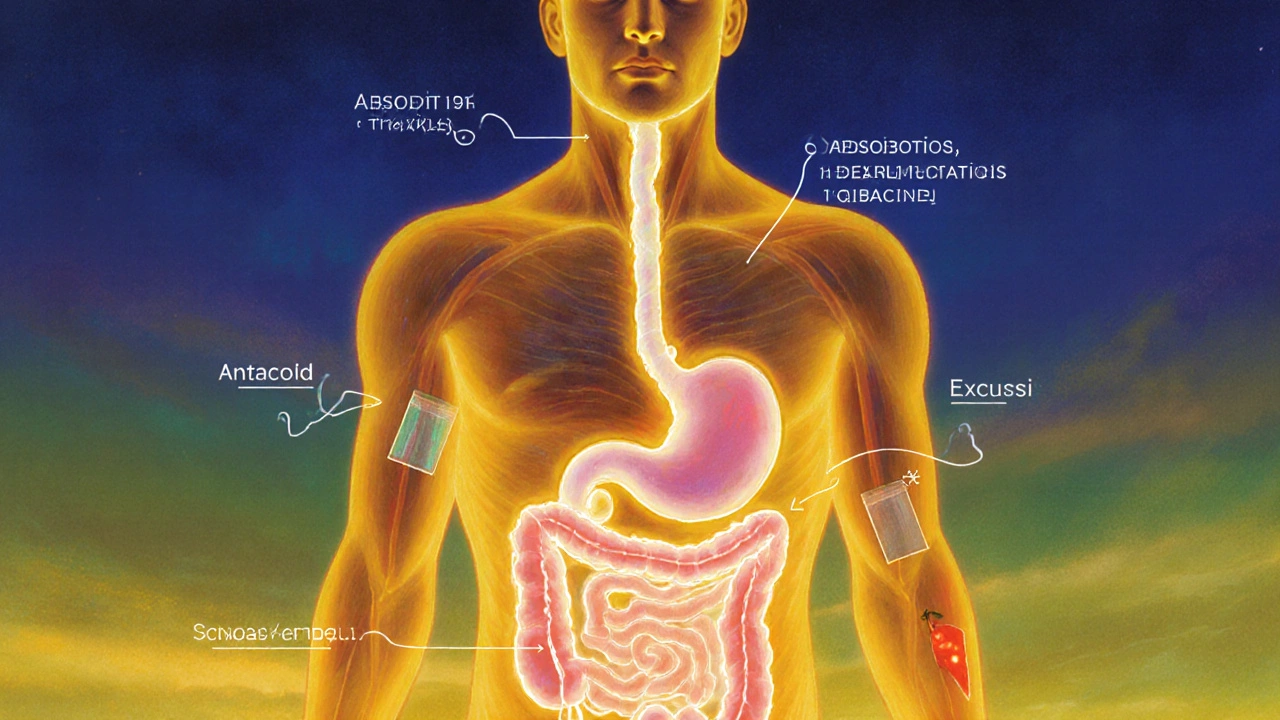
When you take more than one medication, your body doesn’t treat them like separate events—it tries to process them all at once. This is where pharmacokinetic interactions, the way drugs change how your body absorbs, breaks down, or removes other drugs. Also known as drug metabolism interactions, they can make a drug stronger, weaker, or even toxic—without you realizing it. These aren’t just theoretical risks. Real people end up in the ER because their blood thinner stopped working after they started a new antibiotic, or their seizure medication built up to dangerous levels after taking an antifungal.
At the heart of most pharmacokinetic interactions are the CYP450 enzymes, a family of liver proteins that break down over 75% of all prescription drugs. Think of them as your body’s main drug cleaners. Some drugs, like grapefruit juice or the antibiotic clarithromycin, can slam the brakes on these enzymes, causing other drugs to pile up. Others, like the epilepsy drug carbamazepine, can turn them into overachievers—speeding up drug breakdown so your treatment stops working. Warfarin, for example, is especially sensitive. Its metabolism depends heavily on CYP2C9, which is why genetic variants in that enzyme (as covered in our post on warfarin genetics, how inherited differences affect bleeding risk and dosing.) can make your dose wildly unpredictable. Add a common painkiller like ibuprofen, which also affects liver enzymes, and you’ve got a perfect storm.
It’s not just about the liver. Your gut plays a role too. Some drugs change how fast others get absorbed. Others compete for the same transporters in your kidneys, slowing how quickly your body clears them. That’s why transplant patients on tacrolimus need constant monitoring—many common meds, from antifungals to even St. John’s wort, can spike or crash their blood levels. And alcohol? It doesn’t just add drowsiness to benzodiazepines; it changes how your liver handles both drugs, raising overdose risk. These aren’t rare edge cases. They’re everyday clinical realities.
What you’ll find here isn’t just a list of scary warnings. It’s a practical guide to spotting hidden risks. We break down real cases—from how indapamide interacts with other heart meds, to why raltegravir needs special handling during travel, to how Bactrim can throw off your blood sugar if you’re on insulin. You’ll see how these interactions play out in real life, not just in textbooks. No jargon. No fluff. Just what you need to know to keep your meds working—and keep yourself safe.
Pharmacokinetic vs Pharmacodynamic Drug Interactions: What You Need to Know
Learn the difference between pharmacokinetic and pharmacodynamic drug interactions-how they affect your body, why they matter for safety, and what you can do to avoid dangerous side effects.