Insulin Therapy: How It Works and What You Need to Know
When you hear insulin therapy, the medical use of insulin to control blood sugar in people with diabetes. Also known as insulin treatment, it’s a cornerstone of modern diabetes care.
People who need insulin usually have diabetes mellitus, a chronic condition where the body can’t properly regulate glucose levels. In type 1 diabetes the pancreas stops making insulin, while in advanced type 2 the cells become resistant. That’s why insulin therapy becomes essential: it replaces the missing hormone and helps keep glucose within a safe range. There are two main categories – basal (long‑acting) insulin that works like a background thermostat, and bolus (rapid‑acting) insulin that kicks in after meals. Choosing the right mix depends on your daily schedule, eating habits, and how your body responds.
Choosing the Right Insulin Regimen
Delivery options have expanded beyond vials and syringes. Many patients now use pens that let you dial a precise dose with a click, making injections quicker and less messy. For those who want even tighter control, an insulin pump, a small device that delivers continuous insulin through a tiny catheter under the skin can simulate natural insulin release. Pumps can be programmed to give basal rates that vary throughout the day and bolus doses at mealtime, reducing the need for multiple daily shots. However, they require regular skin site changes and a bit of tech‑savvy.
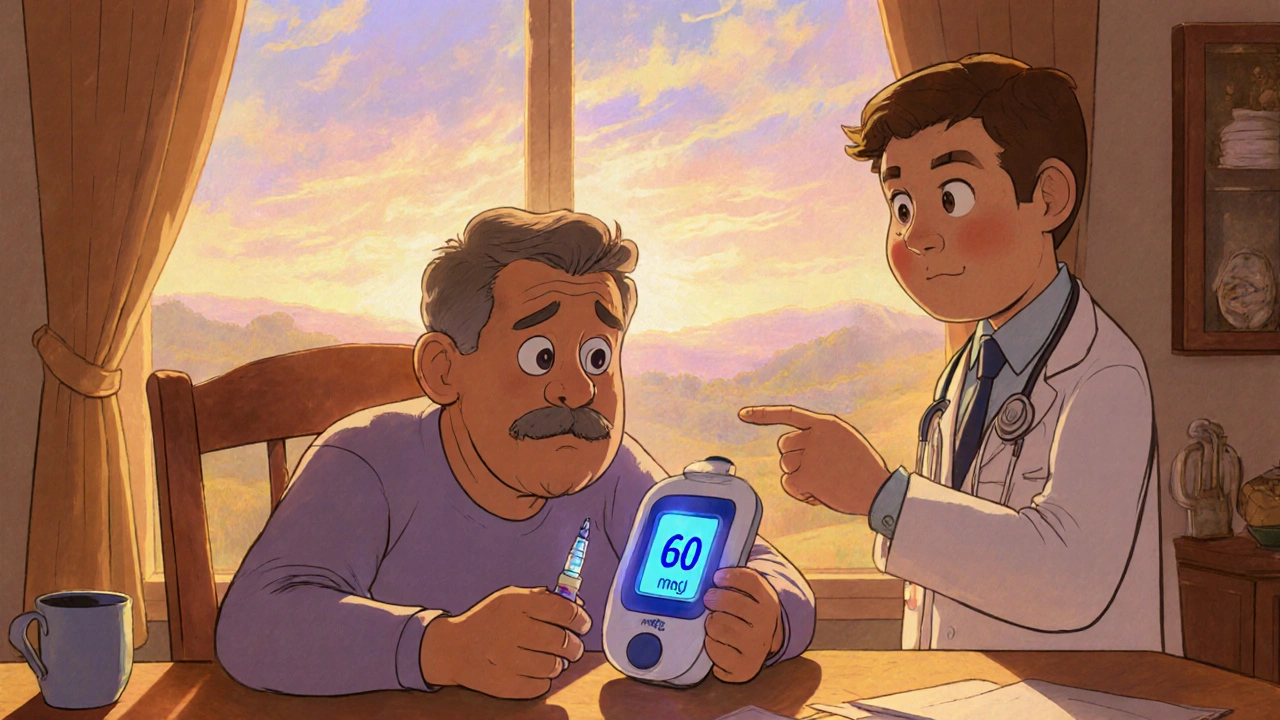
Regardless of the device, you’ll need reliable blood glucose monitoring, the process of checking your blood sugar levels using a meter or continuous sensor. Modern continuous glucose monitors (CGMs) send real‑time data to your phone, alerting you to highs and lows before they become dangerous. Knowing your numbers lets you adjust insulin doses, plan meals, and spot patterns that might signal an issue like hypoglycemia. Speaking of which, low blood sugar is a common side effect of insulin therapy. Symptoms include shakiness, sweating, and confusion, so having fast‑acting carbs on hand is a smart habit.
Nutrition and activity also play big roles. Carbohydrate counting helps you match bolus insulin to what you eat, while regular exercise can boost insulin sensitivity, sometimes letting you use a lower dose. If you’re dealing with both diabetes and mental health challenges, it’s worth noting that stress and mood swings can affect glucose control, so a holistic approach that includes counseling or support groups often pays off.
Below you’ll find a curated list of articles that dive deeper into specific insulin products, compare oral meds with injectable options, and share practical tips for daily management. Whether you’re new to insulin or looking to fine‑tune your regimen, the resources ahead will give you clear, actionable guidance.
Insulin Therapy Side Effects: Managing Hypoglycemia & Weight Gain
Learn why insulin therapy can cause hypoglycemia and weight gain, how to recognize and treat lows, and practical steps to keep weight in check.