Telepharmacy Safety Risk Calculator
Calculate your telepharmacy safety risk score based on key factors from recent studies.
Your Safety Risk Score
Your Safety Report
Risk Factors
Recommendations
When you live in a rural town with no pharmacy within 30 miles, getting your prescriptions filled isn’t just inconvenient-it can be dangerous. Missing doses, delaying refills, or skipping medications altogether becomes common. That’s where telepharmacy comes in. It’s not science fiction. It’s real, it’s growing fast, and by 2025, it’s serving over 40% of U.S. health professional shortage areas. But the big question remains: telepharmacy is expanding access-but is it keeping patients safe?
What Telepharmacy Actually Does
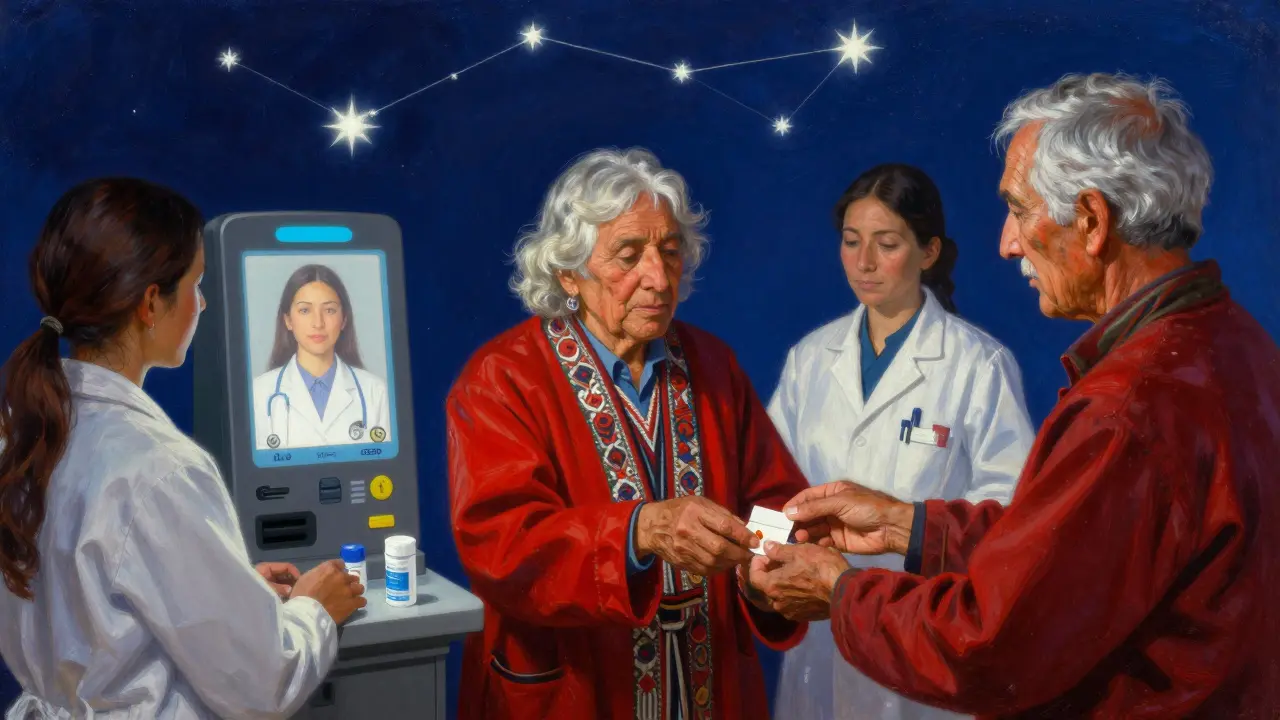
Telepharmacy isn’t just video calls with a pharmacist. It’s a full system: remote dispensing, digital verification, electronic prescriptions, and real-time consultations-all delivered through secure video platforms. Think of it as a pharmacy branch without walls. A central hub, often staffed by licensed pharmacists, connects via high-definition video to remote sites like rural clinics, nursing homes, or even standalone kiosks with automated dispensers.
Two main models dominate: the hub-and-spoke setup, where one pharmacy oversees multiple remote locations, and direct-to-patient services, where pharmacists interact with patients remotely without a physical dispensing location. Both rely on the same core tech: encrypted video, integrated EHRs, automated dispensing machines with remote verification, and backup communication lines. Regulations require at least 720p video quality and HIPAA-compliant data transfer. No flimsy Zoom calls here.
How Safe Is It? The Data
Let’s cut through the noise. A 2021 systematic review by Pathak et al. analyzed six studies from 2010-2020 and found something surprising: telepharmacy matched traditional pharmacies in accuracy. Dispensing error rates? Both hovered between 0.1% and 0.7%. That’s 99.2% to 99.8% accuracy for telepharmacy, compared to 99.3% to 99.9% for brick-and-mortar. Not a statistically meaningful difference.
But safety isn’t just about counting errors. It’s about preventing harm. One 2021 study in Telemedicine and e-Health tracked 3,782 patients over a year. Those with telepharmacy access had a 12.9% increase in hospitalizations due to medication issues. The group without telepharmacy? 40.2%. That’s not a coincidence. When patients can talk to a pharmacist within minutes instead of hours-or days-the risk of dangerous interactions, missed refills, or wrong dosages drops sharply.
Another win: speed. After-hours medication approvals that used to take hours now take 14 to 20 minutes. In emergencies, that’s life-saving. A pharmacist in South Dakota reported catching 1.2 medication errors per 100 prescriptions through remote verification-right in line with traditional pharmacies. That’s not luck. It’s process.
Where Telepharmacy Falls Short
But it’s not perfect. A 2016 study by Skoy et al. found pharmacy students performed consultations 15-20% less effectively via telepharmacy than in person. Why? Non-verbal cues matter. A patient’s shaky hands, slurred speech, or avoiding eye contact can signal confusion, misuse, or adverse reactions. Remote pharmacists can’t see those signs unless they’re trained to look for them-and most aren’t yet.
One Reddit user from North Dakota shared a scary story: a poor video connection led to a missed insulin allergy alert. The result? An adverse reaction. Technical glitches aren’t theoretical. A 2022 survey found 35% of telepharmacy sites struggled with unreliable video or audio. If your connection drops during a high-risk medication review, what happens?
And then there’s training. Not all telepharmacy sites invest in it. Sites with comprehensive technician training saw 22% fewer dispensing errors than those that didn’t. That’s not a small gap. It’s the difference between a safe system and a risky one.

Who Benefits the Most?
The biggest win for telepharmacy isn’t error rates-it’s access. Before 2020, over 10 million Americans lived in pharmacy deserts. A 2023 study in JAMA Network Open showed that states with strong telepharmacy policies cut pharmacy deserts by 4.5% in just one year. Populations without nearby pharmacies shrank by 11.1%. That’s not a marginal improvement. That’s transformative.
Take the Indian Health Service’s program for Navajo Nation communities. They implemented dual verification for high-risk drugs like warfarin and opioids. They also built in a rule: if a case is too complex, it’s instantly transferred to an in-person pharmacist. Result? A medication error rate of 0.45%, below the national average of 0.67%. This isn’t luck. It’s intentional design.
What’s Changing in 2025?
Telepharmacy is evolving fast. In November 2022, CMS expanded Medicare Part D reimbursement for telepharmacy services-meaning more seniors can access it. In January 2023, the FDA launched its Sentinel Initiative to actively track adverse drug events tied to telepharmacy. And the Patient-Centered Outcomes Research Institute (PCORI) is funding a $3.2 million, three-year randomized trial across 12 rural communities. This is the first large-scale, gold-standard study to compare safety outcomes head-to-head.
Artificial intelligence is stepping in too. Companies like MedsAI have raised $22 million to build AI tools that predict adverse drug events before they happen. Early trials show an 18.7% improvement in detection. Imagine a system that flags a dangerous interaction between a new blood pressure med and a patient’s existing diabetes drug-even before the pharmacist reviews it.
By 2026, industry analysts predict telepharmacy will reach safety parity with traditional pharmacies. But there’s a catch: broadband access. Rural areas with poor internet will keep falling behind. Until connectivity improves, safety gaps will persist.
What Needs to Happen Next
The American Pharmacists Association has set a goal: establish evidence-based safety standards for telepharmacy by 2025. That’s critical. Right now, rules vary wildly by state. Twenty-eight states have clear telepharmacy laws. Twenty-two don’t. That’s a patchwork quilt of safety.
Three things need to happen:
- Standardize training. Pharmacists and technicians need 16-24 hours of certified training in remote assessment, tech use, and emergency protocols.
- Require dual verification for high-risk medications. No exceptions.
- Build in automatic escalation. If a case is too complex, the system must route it to an in-person pharmacist immediately.
And we need more data. Not just error counts. We need real-world outcomes: ER visits avoided, hospitalizations prevented, adherence rates improved. Right now, most studies are observational. We need randomized trials-and we’re finally getting them.
Final Thoughts
Telepharmacy isn’t a replacement for traditional pharmacy. It’s a lifeline. For people in rural towns, nursing homes, or places with no pharmacist for miles, it’s the only way to get safe, timely care. The data shows it’s as accurate as a brick-and-mortar pharmacy. It’s faster. It’s saving lives.
But it’s not flawless. Poor tech, weak training, and lack of oversight can turn a helpful tool into a risky one. The difference between success and failure? Intentionality. Systems designed with safety as a priority-like the Navajo Nation program-deliver results. Systems that cut corners don’t.
The future of telepharmacy isn’t about replacing pharmacists. It’s about scaling their expertise. And if we get the standards right, it could be the most important advancement in medication safety since electronic prescribing.
Is telepharmacy as safe as a regular pharmacy?
Yes, when properly implemented. Studies show telepharmacy matches traditional pharmacies in dispensing accuracy, with error rates below 1%. However, safety depends on technology reliability, staff training, and protocols. Poor video quality or untrained staff can increase risk.
Can telepharmacy detect medication misuse?
It can, but with limitations. Pharmacists can spot verbal cues like confusion or hesitation. But they can’t observe physical signs like tremors, slurred speech, or skin changes without in-person exams. Some systems now use AI to flag risky patterns, but human oversight is still essential.
What states allow telepharmacy?
As of 2025, 28 states have specific telepharmacy regulations, including requirements for video quality, data security, and pharmacist licensing. Another 22 states lack clear rules, creating legal uncertainty. The trend is moving toward broader adoption, especially after Medicare expanded reimbursement in 2022.
Does telepharmacy work for complex medications like insulin or warfarin?
Yes, but only with safeguards. Programs like the Indian Health Service’s use dual verification for high-risk drugs and automatically transfer complex cases to in-person pharmacists. When protocols are strict, error rates drop below the national average. Without those safeguards, the risk increases.
Are telepharmacy services covered by insurance?
Medicare Part D now covers telepharmacy services as of November 2022. Many private insurers follow suit, especially in rural states. Coverage varies, but reimbursement is expanding rapidly due to proven access improvements and cost savings from reduced hospitalizations.
What’s the biggest risk with telepharmacy?
The biggest risk is inconsistent implementation. Poor internet, untrained staff, lack of backup systems, and no protocols for complex cases can turn a helpful service into a dangerous one. Safety isn’t built into the tech-it’s built by the people using it.

Cara Hritz
December 22, 2025 AT 14:32Sam Black
December 22, 2025 AT 22:00Jamison Kissh
December 24, 2025 AT 20:59Johnnie R. Bailey
December 25, 2025 AT 23:56Tony Du bled
December 26, 2025 AT 11:11Kiranjit Kaur
December 27, 2025 AT 11:53Gabriella da Silva Mendes
December 28, 2025 AT 10:10Tarun Sharma
December 30, 2025 AT 09:24Johnnie R. Bailey
January 1, 2026 AT 04:30