Anticholinergic Burden Calculator
Calculate Your Medication Risk
Imagine taking a pill for an overactive bladder, only to find yourself unable to pee at all. No warning. No gradual buildup. Just sudden, painful complete blockage. That’s not rare - it’s a documented risk of common medications millions take every day. Anticholinergic drugs, often prescribed for overactive bladder, Parkinson’s, depression, or allergies, can shut down your bladder’s ability to contract. And if you’re a man over 65 with even mild prostate enlargement, your risk jumps from less than 1% to nearly 5%. This isn’t a theoretical concern. It’s happening in real time, in clinics and emergency rooms across Australia, the U.S., and Europe.
How Anticholinergics Break the Bladder’s Signal
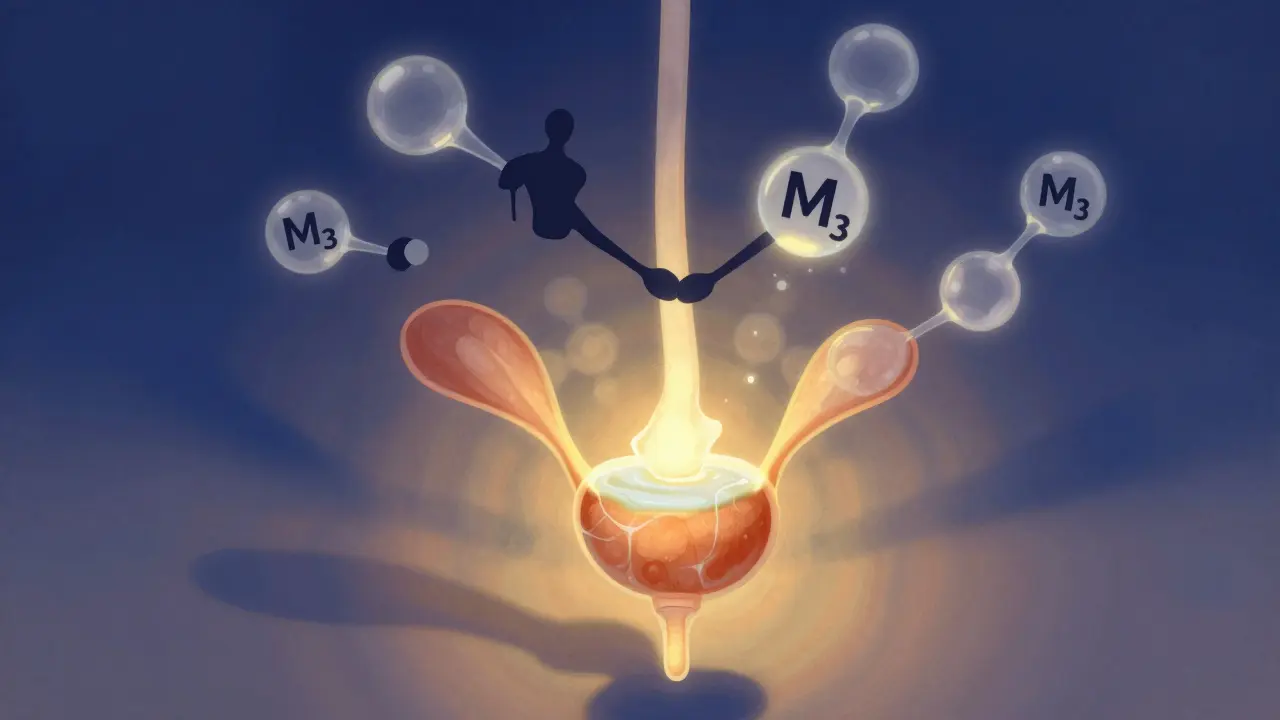
Your bladder doesn’t work like a simple water balloon. Emptying it requires a precise chemical handshake between nerves and muscle. Acetylcholine, your body’s natural signal, binds to M3 receptors on the detrusor muscle - the muscle that squeezes to push urine out. Anticholinergic drugs block those receptors. No signal. No squeeze. Urine stays trapped. It’s not just about the bladder. The whole urinary system depends on balance. The internal sphincter needs to relax. The external sphincter needs to release. Anticholinergics disrupt all of it. Even if your prostate isn’t enlarged, these drugs can still cause retention. But if you have BPH - benign prostatic hyperplasia - you’re already fighting a narrowed urethra. Add an anticholinergic, and you’re stacking two blockades on top of each other. The Urology Textbook (2023) explains that while M2 receptors make up 80% of bladder receptors, only M3 triggers contraction. That’s why drugs targeting M3 specifically - like darifenacin or solifenacin - were developed. But even those aren’t risk-free. Non-selective drugs like oxybutynin, which hit M1, M2, and M3, are the worst offenders. A 2009 NEJM Journal Watch analysis found men with BPH on oxybutynin had over 3 times the risk of retention compared to placebo.Who’s Most at Risk?
It’s not just older men. But they’re the most vulnerable. A 2019 University of Calgary review found that in men over 65 with BPH, anticholinergic use increases urinary retention risk to 4.3%. For women, the risk is lower - around 5% - but still real. Why the difference? Prostate size. Even a slightly enlarged prostate adds resistance. When the bladder muscle can’t generate enough force to overcome it, retention follows. The American Geriatrics Society Beers Criteria (2019) lists anticholinergics as “potentially inappropriate” for older adults - not because they’re useless, but because the risks often outweigh the benefits. In people with dementia, a 2016 JAMA Internal Medicine study showed anticholinergic use increased retention risk by 49%. And it’s not just one drug. When you take multiple anticholinergics - say, an antihistamine for allergies, an antidepressant, and a bladder pill - your total “anticholinergic burden” adds up. The ACB scale scores drugs from 1 to 3. A score of 3 or higher? That’s a 68% increased chance of retention in seniors, according to a 2017 study in the Journal of the American Geriatrics Society.Which Drugs Carry the Highest Risk?
Not all anticholinergics are created equal. Here’s how they stack up:| Drug | Receptor Target | Risk Level (in men with BPH) | Incidence of Retention |
|---|---|---|---|
| Oxybutynin | M1, M2, M3 (non-selective) | High | 1.8-2.5% |
| Trospium chloride | M1, M3 (limited brain penetration) | Moderate-High | 1.5-2.2% |
| Solifenacin | M3-selective (31x over M2) | Moderate | 1.2-1.8% |
| Tolterodine | M3-selective | Low-Moderate | 0.9-1.4% |
| Darifenacin | M3-selective | Low-Moderate | 0.8-1.3% |
Even within this class, the differences matter. Oxybutynin - once the go-to - now has the highest retention risk. Solifenacin and darifenacin are safer, but not safe. And if you’re on a patch? Oxybutynin’s transdermal form cuts retention risk by 42% compared to the pill. Why? Less drug hits your bloodstream all at once.
What Happens When It Goes Wrong?
Acute urinary retention means you can’t pee at all. Your bladder swells. Pain builds. You might feel pressure, nausea, or even vomiting. It’s an emergency. Catheterization is needed. In 2021, the U.S. healthcare system spent $417 million on ER visits and catheterizations for drug-induced retention alone. Chronic retention is sneakier. You can pee - but not fully. You feel like you’re never done. You dribble. You wake up five times a night. Your post-void residual (PVR) - the leftover urine - climbs above 100mL. Over time, this stretches the bladder, weakens the muscle, and can lead to kidney damage. Real stories back this up. On Drugs.com, a 68-year-old man wrote: “After two weeks of oxybutynin, I couldn’t pee. Got catheterized. My urologist said this happens in 1 in 50 men my age with even mild prostate issues.” Reddit’s r/urology has over 120 posts since 2020 describing similar emergencies. A 2022 survey by the National Association for Continence found 8.7% of anticholinergic users needed catheterization - and 63% of those cases happened within the first 30 days.How Doctors Should Prevent This
It’s not about avoiding these drugs entirely. It’s about managing the risk. The American Urological Association (2022) says: Always check your post-void residual before starting an anticholinergic. If your PVR is over 150mL, don’t start. Period. If you’re a man over 65 with prostate symptoms, your doctor should be using a bladder scanner - a non-invasive ultrasound device - to measure how much urine you’re leaving behind. It takes 8 minutes. It’s standard. And yet, many clinics skip it. A 2020 Practice Management study found that only 61% of urologists consistently check PVR before prescribing. If you’re already on one of these drugs, get checked every month for the first three months. Then quarterly. If your residual starts climbing - say, from 80mL to 160mL - your dose should be lowered or stopped. One user on HealthUnlocked said: “My urologist checks PVRs monthly. I’ve been on solifenacin 18 months without issues because we caught a rise at 150mL and cut my dose.”
What Are the Alternatives?
There are better options - especially for men. Mirabegron (Myrbetriq) is a beta-3 agonist. Instead of blocking signals, it boosts the bladder’s natural relaxation pathway. In the 2012 ROSE trial, retention risk was just 0.3% - compared to 1.7% for anticholinergics. It’s now the first-line choice for men with BPH and overactive bladder. OnabotulinumtoxinA (Botox) injections into the bladder wall relax the muscle for months. Retention risk? Only 0.5%. But it requires a specialist and a catheter for a few days after. Peripheral neuromodulation - tiny devices that stimulate nerves near the tailbone - works for about 70% of patients. No pills. No injections. Just a small implant. And now, new tools are emerging. The Anticholinergic Risk Calculator (ARC), launched in 2023, uses age, prostate size, baseline PVR, and other meds to predict your personal risk with 89% accuracy. Genetic testing for CHRM3 receptor variants is also in early use - some people are born with receptors that are extra sensitive to anticholinergics.What You Should Do Now
If you’re taking an anticholinergic for bladder issues:- Ask your doctor: “What’s my post-void residual?” If they don’t know, insist on a bladder scan.
- Are you over 65? Do you have trouble starting your stream? Do you feel like you never finish? These are red flags.
- Check your pill bottle. Is it oxybutynin? If yes, ask about switching to mirabegron or another alternative.
- Are you on more than one anticholinergic? A cold medicine? An antidepressant? A sleep aid? Add up the burden. Use the ACB scale (search “ACB scale drug list” - many are free).
- Don’t wait for symptoms. If you haven’t urinated in 12 hours, go to the ER. Don’t call your doctor. Don’t wait. This is an emergency.
For women, anticholinergics are still often first-line - but even then, PVR checks should be routine. For men? They’ve been pushed to third-line. That’s not because they’re ineffective. It’s because the cost of one retention episode - pain, catheter, infection, hospital stay - far outweighs the benefit of a slightly drier bladder.
Why This Isn’t Just a “Side Effect”
We call it a side effect. But urinary retention isn’t a rash or a dry mouth. It’s a mechanical failure. A life-altering event. A trip to the ER. A catheter. A week of discomfort. A potential kidney injury. The FDA added black box warnings in 2019. The European Medicines Agency banned these drugs in people with prior retention. The American Urological Association says they’re “absolutely contraindicated” in men with a history of retention. Yet, in 2022, over 15 million Americans were still prescribed anticholinergics for overactive bladder. The market is shrinking - mirabegron now holds 31% of prescriptions, while oxybutynin’s share has dropped to 18%. That’s progress. But not enough. This isn’t about avoiding medication. It’s about choosing wisely. Your bladder doesn’t have a backup plan. If the signal gets blocked, it stops working. And sometimes, it never recovers.Can anticholinergic drugs cause permanent bladder damage?
Yes, if urinary retention is chronic and untreated. When the bladder is stretched too long from holding too much urine, the muscle can weaken permanently. This is called detrusor underactivity. Once that happens, you may need lifelong catheterization or surgery. That’s why catching retention early - with PVR checks - is critical.
Are over-the-counter antihistamines linked to urinary retention?
Yes. Diphenhydramine (Benadryl), chlorpheniramine, and even some sleep aids like doxylamine have strong anticholinergic effects. If you’re over 65 or have prostate issues, even one OTC pill a day can add to your total anticholinergic burden. The ACB scale gives these drugs a score of 2 or 3. Combine them with a bladder pill, and your risk spikes.
Why do women have lower risk than men?
Women don’t have a prostate. The urethra is wider and less likely to be mechanically blocked. So even if the bladder muscle is weakened by anticholinergics, urine can still flow out. But women aren’t immune - especially if they’ve had pelvic surgery, nerve damage, or severe prolapse. The risk is lower, but still real.
Is there a safe dose of anticholinergics for men with BPH?
No. Dr. Howard B. Goldman, a leading urologist, stated in the 2020 AUA Guidelines that “no level of anticholinergic exposure is safe in men with prior retention episodes.” Even low doses can trigger retention in susceptible individuals. The risk isn’t linear - it’s threshold-based. Once your bladder is already struggling, even a tiny block on the signal can push you over the edge.
Can I stop anticholinergics cold turkey?
Never stop abruptly without talking to your doctor. If you’re on these drugs for depression, Parkinson’s, or severe incontinence, stopping suddenly can cause withdrawal symptoms or make your original condition worse. But if you’re on them for overactive bladder - and especially if you’re male over 65 - ask your doctor about switching to mirabegron or another safer option. There’s no need to suffer in silence or risk an emergency.
Beth Cooper
January 30, 2026 AT 20:48Melissa Cogswell
January 31, 2026 AT 22:58Lily Steele
February 2, 2026 AT 16:43Bobbi Van Riet
February 2, 2026 AT 17:20Diana Dougan
February 3, 2026 AT 18:44Donna Fleetwood
February 4, 2026 AT 22:27Sazzy De
February 5, 2026 AT 00:24Kathleen Riley
February 5, 2026 AT 20:14Rohit Kumar
February 7, 2026 AT 05:27Shubham Dixit
February 7, 2026 AT 14:57