Weight Gain: Understanding the Why and How
When you hear Weight Gain, the increase in body mass caused by fat, muscle, fluid, or other tissue comes up, you might think of diet or exercise alone. In reality, medications, drugs that can trigger weight changes as side effects play a big role, and so do shifts in appetite, the drive to eat, which can be altered by health conditions or treatments. Even fluid retention, the buildup of excess water in tissues, can add pounds without extra fat. Understanding these pieces helps you spot the real drivers behind the scale moving upward.
First, let’s talk about the link between weight gain and the medicines you might be taking. Many drugs—like certain antipsychotics, steroids, and some antidepressants—can boost hunger signals or slow down metabolism. For example, a drug often used for rheumatoid arthritis may raise calorie intake, while a blood pressure medicine might cause fluid buildup. Knowing which prescription or over‑the‑counter product influences your weight lets you talk to your doctor about alternatives or dosage tweaks before the pounds pile on.
How Metabolism and Appetite Interact
Metabolism is the body’s engine that burns calories, and appetite is the fuel gauge. Some conditions, such as depression or chronic pain, dim the engine and turn up the gauge, leading to extra calories stored as fat. On the flip side, certain antibiotics or anti‑inflammatory meds can temporarily speed up metabolism, but the appetite boost that follows often outweighs the burn. When you track both how fast you’re burning and how much you’re wanting to eat, you get a clearer picture of why weight might creep up even if you haven’t changed your meals.
Fluid retention adds another twist. Medications that affect kidney function or heart health can cause your body to hold onto water, especially if you’re also dealing with heart‑related issues. This isn’t true fat gain, but the scale will still show extra pounds. Reducing sodium, staying active, and monitoring blood pressure are practical ways to keep fluid‑related weight gain in check.
Nutrition plays a starring role, too. For patients with Alzheimer’s or diabetes, the right diet can protect brain health and stabilize blood sugar, both of which affect weight. Simple steps—like swapping refined carbs for fiber‑rich veggies—help keep appetite steady and metabolism humming. In many of the articles below, you’ll see how specific nutrients support weight control while tackling other health challenges.
Exercise isn’t a magic fix, but it can offset medication‑induced weight changes. Even modest activity, such as short walks or yoga poses for muscle spasm relief, improves insulin sensitivity and reduces fluid swelling. When paired with medication reviews, a realistic workout plan makes a noticeable dent in unwanted pounds.
Managing weight gain often means juggling several factors at once. Start by listing any drugs you’re on, then check their side‑effect profiles for weight impact. Next, monitor how your appetite behaves day to day—note cravings, timing, and portion sizes. Finally, watch for signs of fluid retention like swelling in ankles or sudden weight jumps. This three‑step audit gives you concrete data to discuss with a health professional.
The articles in this collection dive into each of these angles. You’ll find detailed comparisons of drugs that commonly cause weight changes, practical guides for handling appetite swings, and strategies to reduce fluid buildup. Whether you’re concerned about a specific prescription, want to understand how lifestyle tweaks can offset side effects, or need a quick overview of nutrition tips for weight control, the posts below have you covered.
Take a look at the full list to see how each topic ties back to the core idea of managing weight gain. The insights will help you make informed choices, ask the right questions at your next appointment, and build a plan that fits your life.
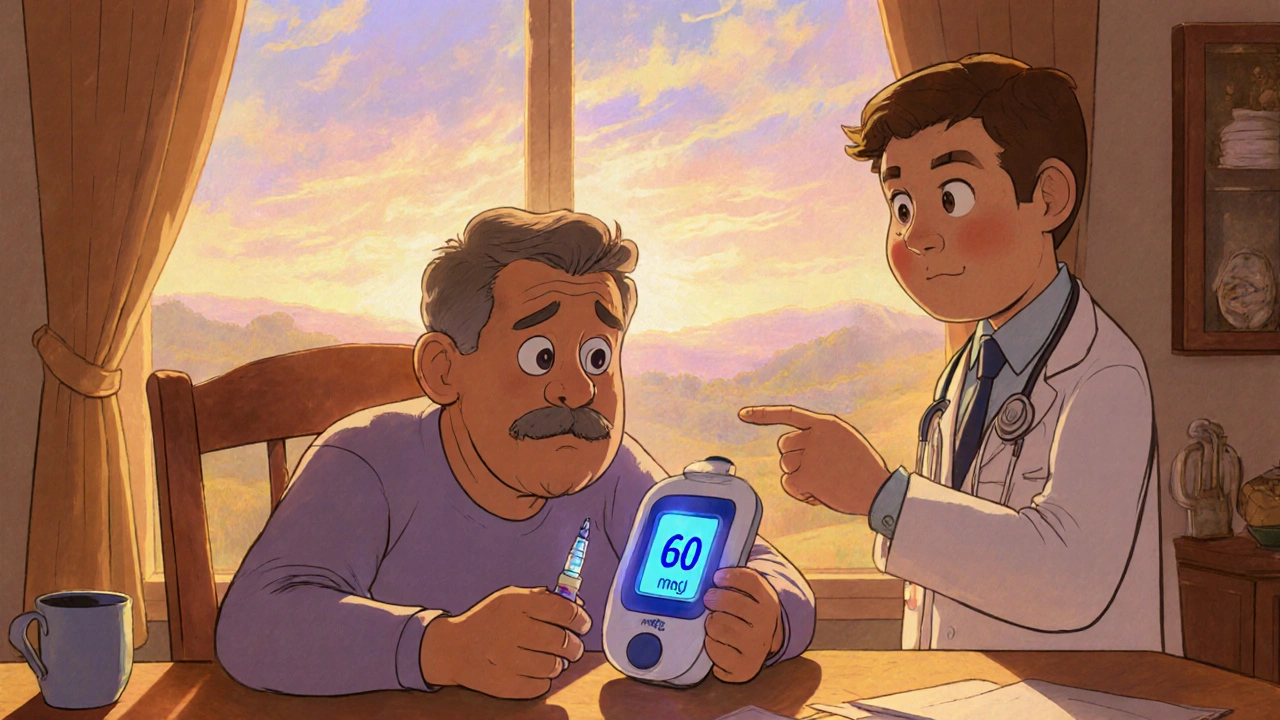
Insulin Therapy Side Effects: Managing Hypoglycemia & Weight Gain
Learn why insulin therapy can cause hypoglycemia and weight gain, how to recognize and treat lows, and practical steps to keep weight in check.