Fluid Retention: Causes, Management, and What to Watch For
When working with Fluid retention, the buildup of extra fluid in body tissues that causes swelling, often in the legs, ankles, or abdomen. Also known as edema, it can be a sign of an underlying health issue or a side effect of medication. Understanding fluid retention means looking at what triggers it, how the body reacts, and which tools help bring balance back.
One of the most common triggers is Sodium intake, the amount of salt you consume each day, which pulls water into the bloodstream and tissues. High‑salt meals raise blood volume, stretch capillaries, and set the stage for swelling. Reducing table salt, processed foods, and salty snacks often shows quick results, especially when paired with proper hydration.
When excess fluid builds up, doctors often turn to Diuretics, medicines that increase urine production to flush out extra water and electrolytes. Common classes include loop diuretics like furosemide and thiazides such as hydrochlorothiazide. These drugs are the frontline response for conditions that push fluid into the interstitial space, but they require monitoring of potassium and kidney function.
Underlying chronic diseases are another major piece of the puzzle. Heart failure, a condition where the heart cannot pump blood efficiently, leading to fluid backup in the lungs and legs creates pressure that forces fluid out of blood vessels and into surrounding tissue. Managing heart failure with lifestyle changes, ACE inhibitors, and appropriate diuretics directly reduces the swelling burden.
Kidney disease also forces the body to hold onto water because the filters that normally excrete it become less effective. When glomerular filtration drops, sodium and fluid retention rise, feeding the same cycle of edema. In these cases, low‑protein diets and careful medication dosing become essential alongside diuretic therapy.
Some prescription drugs can unintentionally trigger swelling. Steroids, certain antidepressants, and even blood pressure pills like calcium channel blockers may increase capillary permeability or retain salt. If you notice new puffiness after starting a medication, a quick chat with your pharmacist or doctor can help you adjust the regimen before swelling worsens.
Practical Steps to Keep Fluid in Check
Start by tracking your daily salt consumption; aim for less than 2,300 mg, and under 1,500 mg if you have heart or kidney concerns. Elevating swollen limbs, wearing compression stockings, and moving around regularly help push fluid back toward the heart. Weigh yourself each morning—tiny weight changes can signal fluid shifts that need medical attention.
Finally, stay hydrated with water, not sugary drinks. paradoxically, drinking enough water tells your kidneys they don’t need to hold onto extra fluid. Pairing these habits with any prescribed diuretics or dietary advice creates a coordinated plan that tackles swelling from multiple angles.
Below you’ll find a curated list of articles that dive deeper into the meds, conditions, and lifestyle tweaks mentioned here. Whether you’re looking for safe ways to purchase a diuretic online, want to understand how a drug like spironolactone interacts with alcohol, or need clear guidance on managing the fluid‑related side effects of other prescriptions, the posts ahead give actionable insight you can use right away.
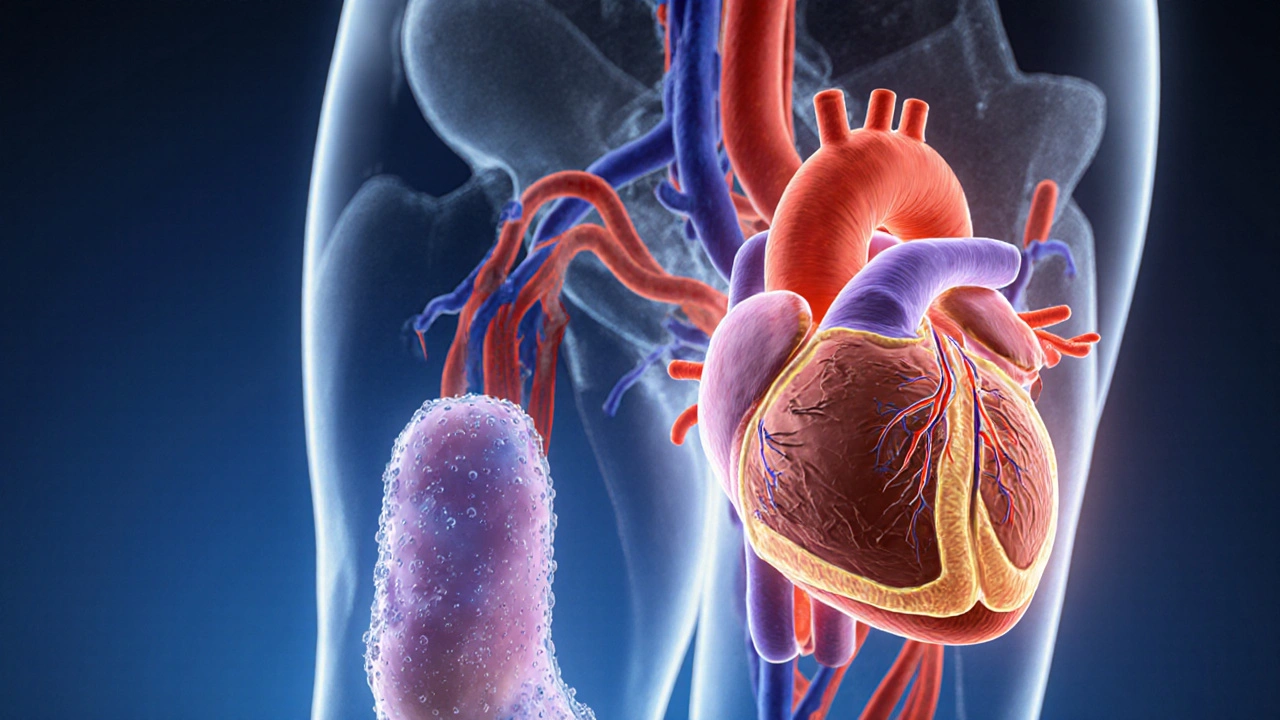
How Fluid Retention Affects Your Heart Health
Explore how fluid retention impacts heart health, recognize warning signs, and learn practical steps to reduce swelling and protect your cardiovascular system.