Fluid Retention & Heart Health Risk Calculator
Please answer the following questions to assess your risk of fluid retention affecting your heart health.
This calculator helps assess your risk of fluid retention affecting your heart health based on common lifestyle factors and symptoms. Scores range from Low Risk to High Risk.
Higher scores suggest a greater need for monitoring and lifestyle adjustments.
This tool provides general guidance only. It is not a substitute for professional medical advice. Consult a healthcare provider for accurate diagnosis and treatment.
Your Risk Assessment
Key Takeaways
- Fluid retention (edema) can raise blood pressure and force the heart to work harder.
- Kidney function, sodium intake, and inflammation are the main drivers linking swelling to heart strain.
- Early signs include swollen ankles, sudden weight gain, and shortness of breath.
- Lifestyle tweaks-less salt, regular movement, and proper hydration-can ease fluid buildup and protect the heart.
- Seek medical advice if swelling persists, you have chest pain, or blood pressure spikes.
Understanding Fluid Retention
When your body holds onto excess water, it’s called Fluid Retention is the accumulation of excess fluid in the body's tissues, often visible as swelling or edema. While a temporary puffiness after a long flight is harmless, chronic fluid buildup can signal deeper health issues, especially for the heart.
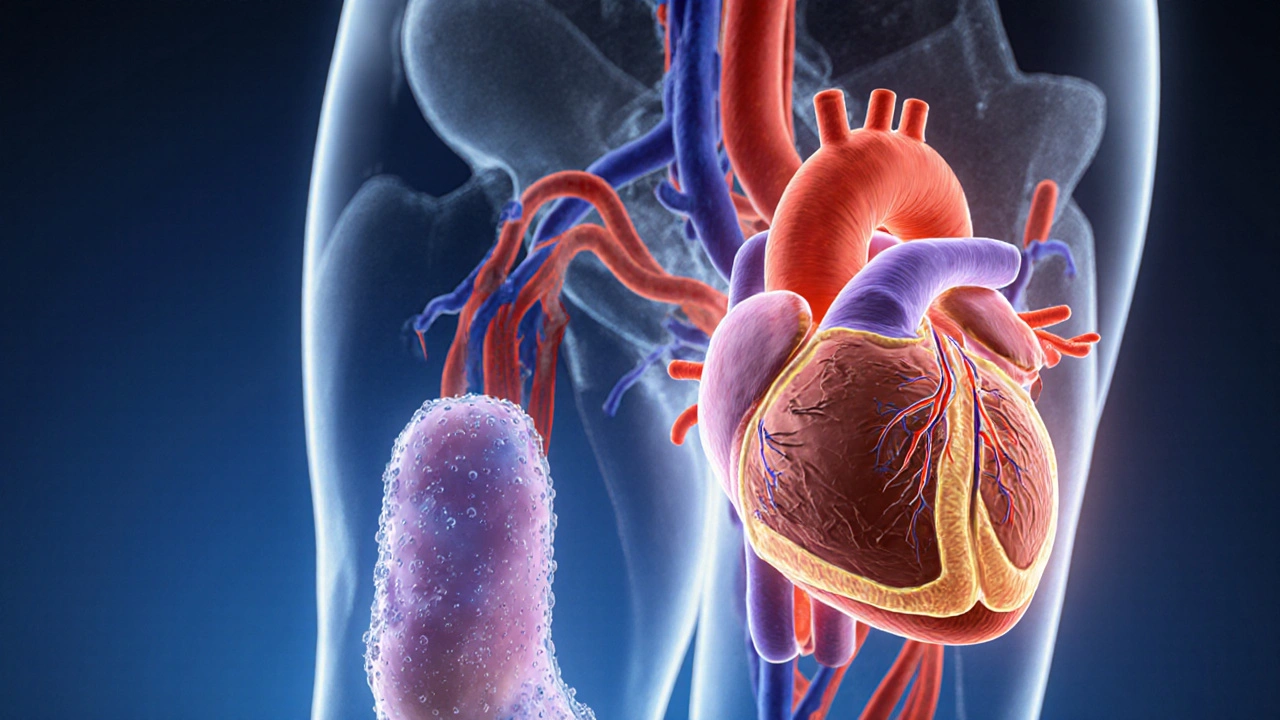
Why the Heart Pays Attention
The heart’s job is to push blood through a network of vessels, delivering oxygen and nutrients. When fluid pools in the legs or abdomen, the blood volume rises, and the heart has to pump against higher pressure. This extra workload can lead to Heart Health is the overall condition of the cardiovascular system, including the heart's ability to pump efficiently and maintain normal rhythm. Over time, the strain can manifest as high blood pressure, atrial enlargement, or even heart failure.
The Physiological Bridge: How Swelling Impacts the Cardiovascular System
Three core mechanisms connect fluid retention to heart stress:
- Increased Blood Volume: Extra water adds to the circulating volume, raising Blood Pressure is the force exerted by circulating blood on the walls of blood vessels. Higher pressure forces the heart to contract more forcefully.
- Kidney Overload: The kidneys regulate fluid balance. When they’re forced to filter a larger volume, they may retain sodium, which pulls even more water into the bloodstream, creating a vicious cycle.
- Inflammatory Signals: Conditions like chronic heart disease release inflammatory hormones that make blood vessels leak, spilling fluid into surrounding tissue.
Key Players That Influence Both Fluid Retention and Heart Function
| Factor | Effect on Fluid Retention | Impact on Heart |
|---|---|---|
| High Sodium Intake | Retains water by increasing extracellular fluid | Elevates blood pressure, makes heart work harder |
| Kidney Disease | Reduces fluid excretion | Leads to volume overload and hypertension |
| Medications (e.g., NSAIDs, steroids) | Cause vasoconstriction and sodium retention | Can trigger or worsen heart failure symptoms |
| Physical Inactivity | Slows lymphatic pumping of excess fluid | Weakens cardiovascular conditioning, raises resting heart rate |
| Hormonal Imbalance (e.g., aldosterone excess) | Promotes sodium and water reabsorption | Raises systemic vascular resistance, stressing the heart |
Spotting the Warning Signs Early
Because fluid retention can develop silently, paying attention to subtle cues is crucial. Common red flags include:
- Swelling in the ankles, feet, or lower legs-especially after standing.
- Sudden weight gain of more than 2kg (4‑5lb) over a few days.
- Shortness of breath during routine activities.
- Feeling unusually tight or “full” in the abdomen.
- Increased nighttime urination (the body tries to get rid of excess fluid).
If you notice any of these alongside chest discomfort or a rapid heartbeat, it’s time to talk to a clinician.
Practical Steps to Reduce Fluid Retention and Protect Your Heart
Below is a straightforward checklist you can start today. Each tip tackles a specific driver of swelling while also easing cardiac load.
- Cut back on salt. Aim for less than 2g of sodium per day (about 1tsp of table salt). Read labels; many packaged foods hide 300‑500mg per serving.
- Stay hydrated. Odd as it sounds, drinking enough water (about 2L daily) helps kidneys flush excess sodium.
- Move every hour. Simple leg lifts or a brief walk activates the calf muscle pump, pushing fluid back toward the heart.
- Elevate swollen limbs. Raising feet on a pillow for 15‑30minutes reduces hydrostatic pressure.
- Eat potassium‑rich foods. Bananas, avocados, and leafy greens counterbalance sodium’s effects on fluid balance.
- Monitor weight daily. A kitchen scale can catch small gains before they become noticeable swelling.
- Limit alcohol and caffeine. Both can promote dehydration followed by fluid retention when you rehydrate.
- Check medications. Talk to your doctor about alternatives if you’re on NSAIDs, certain blood pressure drugs, or steroids.
When to Seek Professional Help
Self‑care works for mild cases, but persistent edema may signal an underlying heart condition. Schedule an appointment if:
- Swelling doesn’t improve after a few days of lifestyle changes.
- You experience chest pain, palpitations, or faintness.
- Your blood pressure stays above 140/90mmHg despite diet tweaks.
- You have a known history of heart disease, kidney problems, or liver cirrhosis.
Doctors can run a simple panel-blood tests, echocardiogram, and urine analysis-to pinpoint the cause and prescribe diuretics or other targeted therapies.
Long‑Term Outlook: Managing Fluid Balance for a Healthy Heart
Research from the American Heart Association (2023) shows that patients who consistently monitor sodium intake and stay active reduce heart‑failure hospitalizations by 30%. Likewise, a 2022 Australian cohort study linked regular leg‑elevation routines with lower rates of peripheral edema in older adults.
The take‑away is clear: fluid retention isn’t just a nuisance; it’s an early warning system for cardiac strain. By treating the swelling, you’re giving your heart a lighter load and a better chance to stay strong for years to come.

Frequently Asked Questions
Can drinking more water actually reduce swelling?
Yes. Adequate hydration helps kidneys flush excess sodium, which in turn pulls water out of the tissues. Aim for about 2liters per day unless otherwise advised by your doctor.
Is edema always a sign of heart failure?
No. Edema can stem from kidney disease, liver issues, medications, or simple prolonged standing. However, persistent or unexplained swelling should be evaluated for cardiac involvement.
How much sodium is considered safe for a healthy adult?
Health experts recommend less than 2grams of sodium per day (about 5grams of salt). Most processed foods exceed this, so reading nutrition labels is essential.
Do diuretics cure fluid retention?
Diuretics help the body expel excess water, but they treat the symptom, not the root cause. Lifestyle changes and managing underlying conditions are still crucial.
Can exercise worsen swelling if I already have edema?
Gentle, low‑impact activity (walking, swimming) usually improves circulation and reduces swelling. High‑intensity workouts might temporarily raise blood pressure, so start slowly and talk to your doctor if you’re unsure.
Artie Alex
October 2, 2025 AT 17:25In the context of cardiovascular homeostasis, the phenomenon of extracellular fluid accumulation-commonly designated as edema-constitutes a pathophysiological perturbation of considerable clinical import. When systolic afterload is elevated secondary to hypervolemia, the myocardium experiences increased wall stress, precipitating maladaptive remodeling. Moreover, the renin-angiotensin-aldosterone axis may be dysregulated, fostering sodium and water retention in a deleterious feedback loop. The interplay between endothelial permeability and lymphatic insufficiency further exacerbates interstitial transudation, thereby amplifying preload. Contemporary epidemiological data suggest that patients with chronic edema exhibit a 27% greater incidence of left ventricular hypertrophy. From a hemodynamic standpoint, the Frank–Starling curve is displaced upward, indicating compromised contractile efficiency. Diagnostic algorithms now integrate bioimpedance spectroscopy to quantify fluid overload with granularity hitherto unattainable. Therapeutic regimens incorporating loop diuretics, aldosterone antagonists, and sodium‑restricted diets have demonstrated synergistic efficacy. Nonetheless, the iatrogenic risk of electrolyte derangements mandates vigilant monitoring of serum potassium and creatinine. In addition, longitudinal adherence to physical activity protocols-particularly calf‑pump exercises-has been shown to augment venous return and mitigate peripheral pooling. It is incumbent upon clinicians to adopt a multimodal approach that harmonizes pharmacologic intervention with lifestyle modification. Failure to address subclinical edema may precipitate overt heart failure decompensation, culminating in hospitalization. Therefore, a proactive surveillance strategy, encompassing daily weight logs and periodic echocardiographic assessment, is advisable. Ultimately, the mitigation of fluid retention serves as a pivotal lever in preserving myocardial integrity and averting adverse cardiovascular events. Consequently, patient education regarding sodium labeling becomes an indispensable component of comprehensive care.
abigail loterina
October 3, 2025 AT 16:00Thanks for breaking that down! It really helps to see how small changes can make a big difference for our hearts.
Roger Cole
October 4, 2025 AT 19:46Keep an eye on your weight daily.
Krishna Garimella
October 5, 2025 AT 23:33Think of your body as a river, constantly flowing and balancing. When excess water sticks around, it’s like a dam building up pressure downstream. That pressure forces the heart to pump harder, and over time the engine can wear out. Simple habits-like sipping water, moving your legs, and cutting back on salty snacks-keep the current smooth. Embrace each step as a mindful act of self‑care, and you’ll nurture both flow and strength.
nalina Rajkumar
October 7, 2025 AT 03:20Totally agree 😊 staying active really helps 💪 and those tiny salt cuts add up
Michael Barrett
October 8, 2025 AT 07:06Indeed, the confluence of neurohormonal activation, renal sodium reabsorption, and peripheral vascular resistance, creates a perfect storm for volume overload; consequently, clinicians must employ a nuanced, evidence‑based algorithm, integrating diuretic titration, dietary counseling, and regular hemodynamic monitoring, to forestall progressive cardiac decompensation!
Inma Sims
October 9, 2025 AT 10:53Oh, absolutely, because nothing says “I care” quite like a spreadsheet of sodium grams next to your morning coffee-truly the height of medical sophistication.
Gavin Potenza
October 10, 2025 AT 14:40Honestly, it’s kinda like life-if you keep stacking on extra stuff, eventually the whole thing’s gonna creak. Lighten the load, and everything runs smoother.
Virat Mishra
October 11, 2025 AT 18:26Ugh this whole thing is just another hype piece, nobody reads this stuff anyway.
Daisy Aguirre
October 12, 2025 AT 22:13Hey, don’t be so down! 🌈 Even a tiny tweak, like swapping fries for a banana, can paint your heart with brighter health colors.
Natalie Kelly
October 14, 2025 AT 02:00Its good 2 check ur weigh daily and keep salt low.
Tiffany Clarke
October 15, 2025 AT 05:46Feeling overwhelmed by all this info but I get it.
Adam Baxter
October 16, 2025 AT 09:33Let’s move more drink water stay active keep heart happy
Keri Henderson
October 17, 2025 AT 13:20Exactly, take charge today-set a timer to stand up every hour and watch the difference.