Edema: What It Is and How to Manage It
When dealing with Edema, the buildup of excess fluid in body tissues that causes swelling. Also known as fluid retention, it isn’t just a cosmetic issue – it can signal deeper health problems. Understanding the why and how behind the puffiness helps you act faster and avoid complications.
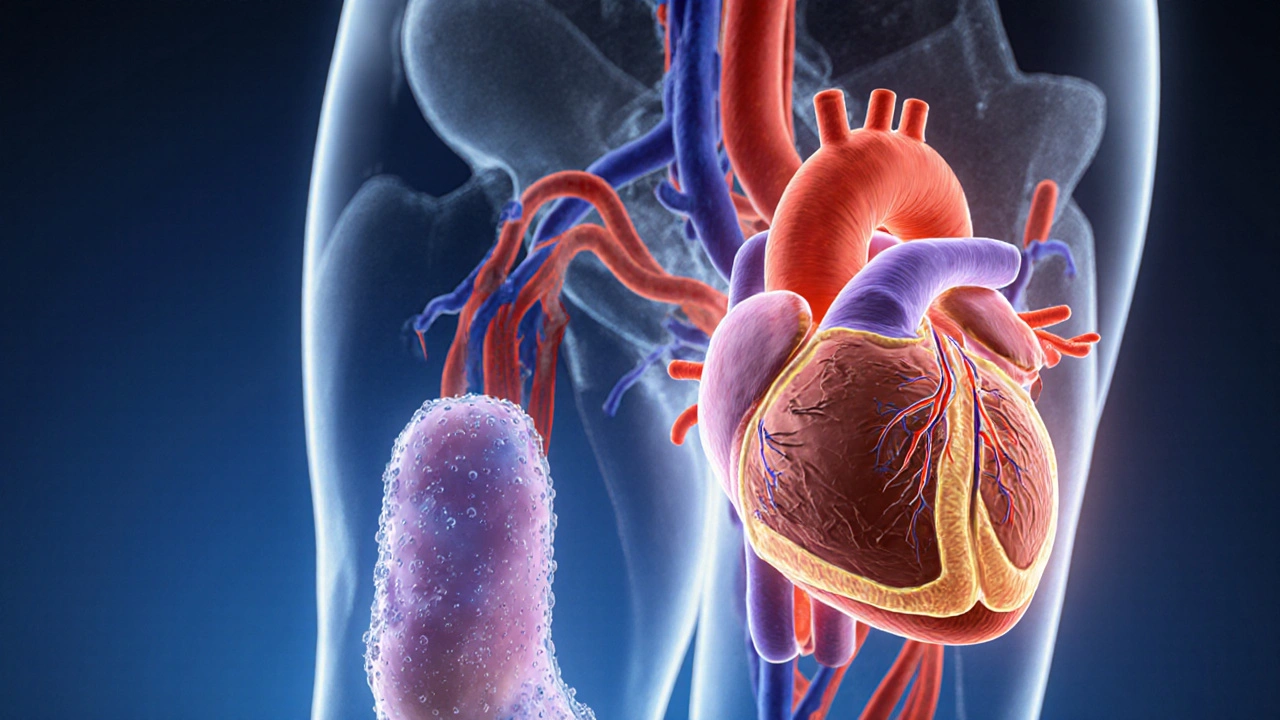
One of the biggest drivers of edema is Heart Failure, a condition where the heart can’t pump blood efficiently. When the heart struggles, blood backs up into the veins, raising pressure and forcing fluid out of the vessels into the legs, abdomen, or lungs. A similar story unfolds with Kidney Disease, damage to the organs that filter waste and fluid from the blood. Impaired kidneys can’t excrete enough water, so the body stores it, leading to visible swelling. These two conditions often overlap—patients with chronic heart problems frequently develop kidney issues, creating a feedback loop that amplifies edema.
Common Triggers and Everyday Factors
Beyond organ failure, several everyday factors can tip the balance toward fluid buildup. Diabetes, a metabolic disorder that affects blood sugar regulation is a frequent culprit because high sugar levels damage tiny blood vessels, reducing their ability to return fluid to the heart. High blood pressure, another diabetes‑related problem, pushes extra fluid out of the arteries. Certain medications also play a role: non‑steroidal anti‑inflammatory drugs (like ibuprofen), calcium‑channel blockers, and even some antidepressants can cause the kidneys to retain sodium, which pulls water along for the ride. The result is that even a modest increase in salt intake can swell your ankles or hands.
Lifestyle choices matter, too. Eating a diet high in processed foods keeps sodium levels high, and sitting or standing for long periods slows the muscle pump that pushes fluid back toward the heart. Simple habits—like elevating the legs, wearing compression stockings, or taking short walks—can keep fluid from pooling. When diet and movement aren’t enough, doctors often turn to Diuretics, medications that increase urine output to reduce excess fluid. These drugs act like a tap, letting the body flush out the extra water while preserving essential electrolytes.
Monitoring is key. Keep an eye on sudden weight gain (more than two pounds in a day), tightening shoes, or a persistent puffiness that doesn’t improve after rest. These signs can indicate that the underlying condition is worsening and may need a medication tweak or further testing. Lab work often includes checking kidney function (creatinine, eGFR) and heart markers (BNP or NT‑proBNP) to pinpoint the source. If you have a known heart or kidney condition, regular check‑ups are non‑negotiable—early detection prevents the swelling from spiraling into dangerous fluid in the lungs or abdomen.
Putting it all together, edema is a symptom that ties together heart health, kidney performance, blood sugar control, medication side‑effects, and lifestyle habits. By recognizing the connections—heart failure leads to fluid backup, diabetes weakens vessel walls, and common drugs can lock sodium in—you can work with your clinician to target the root cause rather than just the surface puffiness. Below you’ll find a curated set of articles that dig deeper into each of these angles, from practical diet tips to how specific meds like spironolactone or NSAIDs affect fluid balance. Use them as a roadmap to keep your body’s fluid levels in check and stay ahead of any flare‑ups.
How Fluid Retention Affects Your Heart Health
Explore how fluid retention impacts heart health, recognize warning signs, and learn practical steps to reduce swelling and protect your cardiovascular system.