Drug Interactions After Transplant: What You Need to Know
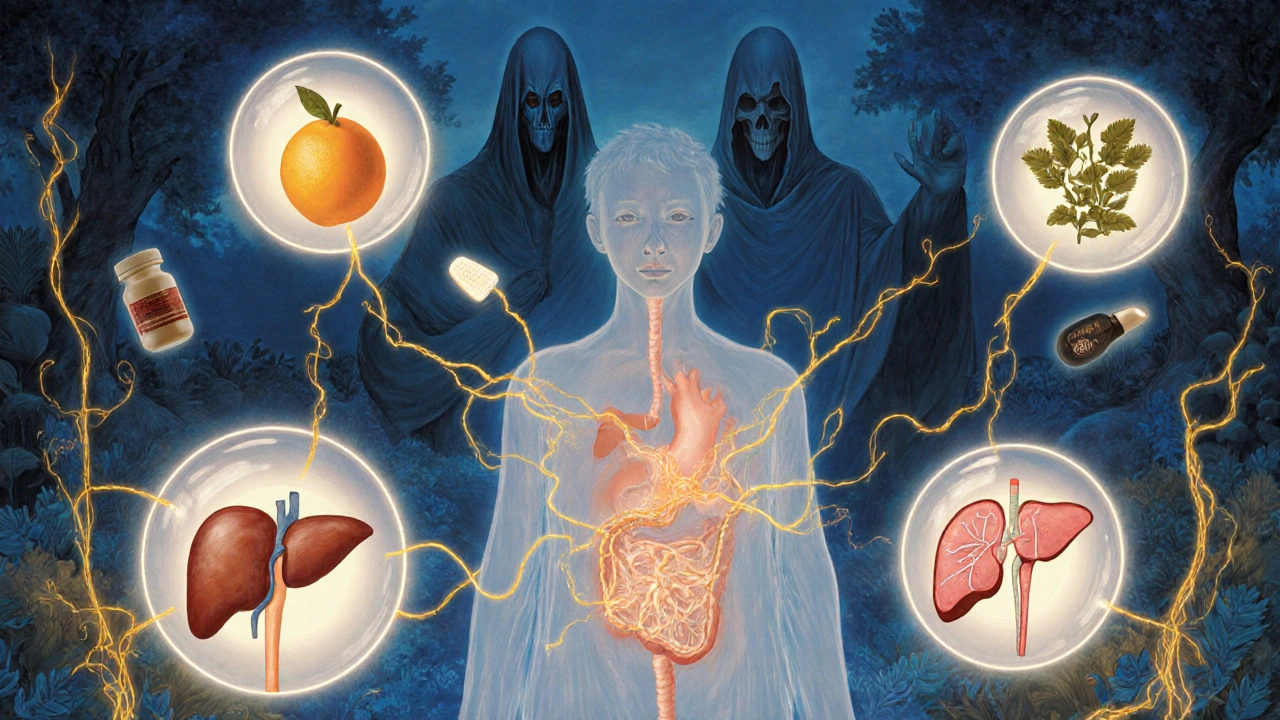
When you’ve had a transplant, a medical procedure where a failing organ is replaced with a healthy one from a donor. Also known as organ transplant, it’s not the end of the journey—it’s just the start of lifelong medication management. Your body doesn’t know the new organ is supposed to be there. So, you take immunosuppressants, drugs that quiet your immune system so it doesn’t attack the transplanted organ. These are non-negotiable. But here’s the catch: these same drugs don’t play well with others. A simple cold medicine, an antibiotic, or even grapefruit juice can throw your whole system out of balance.
Take calcineurin inhibitors, a major class of transplant drugs including tacrolimus and cyclosporine. They’re powerful, but their narrow safety window means even small changes in blood levels can cause kidney damage or rejection. Many common drugs—like certain antibiotics, antifungals, and even some heart meds—can make them too strong or too weak. And if your levels drop? Your body might start rejecting the new organ. If they spike? You could face kidney failure, seizures, or worse.
It’s not just about the transplant drugs themselves. You’re also likely on blood thinners, acid reducers, or cholesterol meds. Each one adds another layer of risk. For example, mixing warfarin with some antibiotics can send your INR through the roof—leading to dangerous bleeding. Or combining statins with certain antifungals? That’s a recipe for muscle breakdown. These aren’t rare edge cases. They happen every day in transplant clinics.
You might think, "I take my meds exactly as prescribed." But what about the over-the-counter stuff? The herbal tea your cousin swears by? The painkiller you grabbed for a headache? These are the hidden traps. Even something as simple as St. John’s wort can make your immunosuppressants useless. And if you’re traveling—like managing raltegravir on a trip—you need to know how time zones, food, and local meds can mess with your regimen.
That’s why so many transplant patients end up in the ER—not because they missed a dose, but because something they added to their routine reacted badly. The good news? You don’t have to guess. Every drug you take should be checked against your transplant meds. Your pharmacist, your transplant team, even your primary doctor—they all need to be on the same page. Keep a list. Update it every time something changes. Ask before you take anything new.
There’s no single rule that fits everyone. Your risk depends on what organ you got, what drugs you’re on, your age, your liver function, even your genetics. But the core truth is simple: drug interactions transplant patients face are among the most dangerous in medicine. They’re silent, they’re common, and they’re often preventable.
Below, you’ll find real, practical guides that break down exactly which drugs clash with transplant meds, how to spot trouble early, what to do if you accidentally mix something dangerous, and how to talk to your care team so nothing slips through the cracks. No fluff. No jargon. Just what you need to stay alive and healthy after your transplant.
Organ Transplant Recipients: Immunosuppressant Drug Interactions and Side Effects
Transplant recipients rely on lifelong immunosuppressant drugs to prevent rejection-but these medications come with serious side effects and dangerous drug interactions. Learn how tacrolimus, mycophenolate, and steroids affect your body, what to avoid, and how to stay safe.