Switching from a brand-name drug to a generic version is supposed to save money-without sacrificing effectiveness. For most people, it works just fine. But for some, a simple change in pill color or shape can trigger headaches, anxiety, seizures, or worse. If you’ve noticed something off after your pharmacy handed you a new bottle of the same medication, you’re not imagining it. And you’re not alone.
Why Switching Generics Can Cause Problems
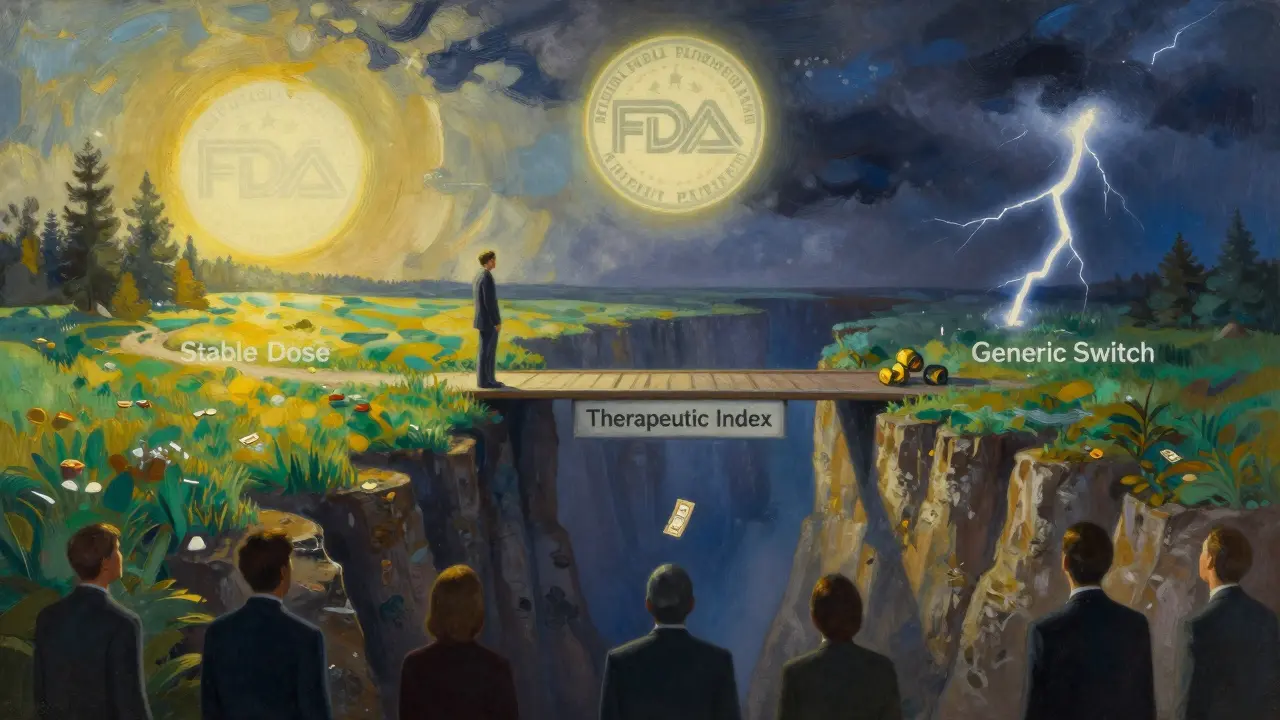
The FDA says generics are bioequivalent to brand-name drugs. That means they must deliver 80% to 125% of the active ingredient into your bloodstream at the same rate. Sounds fair, right? But here’s the catch: that 45% total range of possible variation means two different generics of the same drug can behave very differently in your body. For most medications, that’s fine. For others, it’s dangerous. The real risk comes with drugs that have a narrow therapeutic index-medications where even a small change in blood levels can cause treatment failure or serious side effects. Think seizure meds, thyroid hormones, blood thinners, immunosuppressants, and some psychiatric drugs. In these cases, a 10% drop in absorption might mean your seizure returns. A 15% spike could send your INR levels soaring, putting you at risk for a stroke. A 2019 study in BMJ Open found that patients switching between different generic versions of the same cardiovascular drug had a 12.3% higher chance of being hospitalized within 30 days. That’s not a fluke. It’s a pattern.Which Medications Are Most Likely to Cause Issues?
Not all generics are created equal. Some drug classes are far more sensitive to formulation changes than others. Here are the top five where switching can go wrong:- Antiepileptics (like divalproex sodium, phenytoin): Even small shifts in blood levels can trigger breakthrough seizures. A 2021 survey of 147 neurologists found 68.7% believed generic switches increased seizure risk-and 42.3% had seen it happen in their patients.
- Thyroid medication (levothyroxine): Your body is extremely sensitive to tiny changes in hormone levels. Switching brands can cause fatigue, weight gain, heart palpitations, or even worsen heart disease. The American Thyroid Association recommends sticking with the same manufacturer whenever possible.
- Warfarin: This blood thinner has a razor-thin safety margin. A study showed switching generics led to unstable INR levels in 1 in 5 patients, increasing the risk of clots or bleeding.
- Immunosuppressants (tacrolimus, cyclosporine): After organ transplants, even a 10% drop in drug levels can lead to rejection. Multiple case reports link generic switches to acute transplant failure.
- Extended-release ADHD meds (Adderall XR, Vyvanse generics): Different manufacturers use different bead-release systems. One generic might release the drug too fast, causing jitteriness. Another might release it too slow, making symptoms return by midday. Patients report sudden mood swings, insomnia, and loss of focus within hours of switching.
What Patients Are Saying: Real Stories, Real Consequences
Behind the statistics are real people. On Reddit’s r/ADHD community, a 2022 thread titled “Generic Adderall Switch Ruined My Life” got over 800 comments. Most described the same thing: “I felt fine on my old generic. The new one? I couldn’t focus, I was anxious all day, and I couldn’t sleep.” One person wrote, “I thought I was losing my mind-until I switched back and felt normal again in 48 hours.” A 2023 hospital review of 1,437 patients found that 63.2% of those taking generic ADHD meds noticed reduced effectiveness after a manufacturer change. Nearly half reported new side effects: headaches (28.4%), increased anxiety (22.1%), nausea (19.3%). One patient developed serotonin syndrome after unknowingly taking two different generics at the same time-because the pharmacy switched brands and the old bottle was still in the medicine cabinet. These aren’t anecdotes. They’re patterns confirmed by clinical data.
Why This Keeps Happening
You’d think pharmacies would stick with one generic manufacturer for stability. But they don’t. Pharmacy benefit managers (PBMs)-the middlemen between insurers and pharmacies-repeatedly switch which generic brand is covered based on which one offers the biggest rebate. CVS Caremark, Express Scripts, OptumRx-they all do it. A Senate investigation found PBMs change preferred generic manufacturers an average of 4.7 times per year per drug. That means you could be on one generic in January, a different one in March, another in June. And if you’re on a high-risk medication, each switch is a gamble. Levothyroxine alone has 12 different generic manufacturers approved by the FDA. That’s 12 different formulations. 12 different ways your body might react.What You Can Do: Protect Yourself
You don’t have to accept this as normal. Here’s how to take control:- Check the NDC code. It’s the 11-digit number on your pill bottle. Write it down. If it changes on your next refill, ask why.
- Ask for the manufacturer name. When you pick up your prescription, say: “Can I get the same manufacturer as last time?” Pharmacists can often honor that request-even if it’s not the cheapest option.
- Request ‘Dispense As Written’ (DAW-1). If you’re on a high-risk drug, ask your doctor to write “DAW-1” on your prescription. That legally prevents substitution without your consent.
- Track your symptoms. Keep a simple log: date of refill, manufacturer name, how you felt in the first 72 hours. Did your anxiety spike? Did your energy drop? Did you have a seizure? Write it down. This data helps your doctor.
- Don’t assume “same drug = same effect”. Just because it’s the same active ingredient doesn’t mean it works the same way in your body.
When to Call Your Doctor
If you notice any of these after switching generics, contact your provider right away:- New or worsening side effects (headaches, dizziness, nausea, mood changes)
- Return of symptoms you had under control (seizures, chest pain, fatigue, brain fog)
- Unexplained changes in lab results (INR, TSH, drug levels)
- Feeling “off” for more than 3 days after a refill
The Bigger Picture: A System That Prioritizes Cost Over Care
Generics save the U.S. healthcare system about $165 billion a year. That’s huge. But the cost of switching-related hospitalizations? An estimated $2.1 billion annually. That’s not a savings-it’s a failure of the system. The FDA still insists generics are interchangeable. But clinicians on the ground see the damage. The American College of Clinical Pharmacy and the American Society of Health-System Pharmacists now recommend against automatic substitution for 17 specific drugs-including tacrolimus, bupropion XL, and phenytoin. In 2023, Medicare started limiting generic switches to no more than twice a year for Part D patients. That’s a step forward. But it’s not enough. Until the rebate system changes, patients on high-risk medications need to be their own advocates. Because no algorithm, no rebate, and no FDA guideline can replace the knowledge of how your own body responds to a drug.Can switching to a generic drug really cause side effects?
Yes, for certain medications-especially those with a narrow therapeutic index like antiepileptics, thyroid hormones, blood thinners, and immunosuppressants. Even small differences in how the drug is absorbed can trigger side effects or reduce effectiveness. Many patients report new headaches, anxiety, insomnia, or return of original symptoms after switching generics.
Why do generics sometimes work differently than brand-name drugs?
Generics must contain the same active ingredient, but they can differ in inactive ingredients, coating, and how the drug is released over time. For extended-release pills, different manufacturers use different bead systems or release mechanisms. These differences are allowed under FDA rules (up to 20% variation in absorption), and while they’re safe for most drugs, they can cause problems for medications where precise dosing is critical.
Which drugs are most likely to cause problems when switched to generics?
The highest-risk drugs include antiepileptics (like phenytoin and divalproex), levothyroxine (for thyroid), warfarin (a blood thinner), tacrolimus (for transplant patients), and extended-release ADHD medications like Adderall XR. These drugs have a narrow therapeutic index, meaning small changes in blood levels can lead to serious consequences.
How can I find out which generic manufacturer I’m getting?
Look at the NDC code on your pill bottle-it’s an 11-digit number. You can search this code online using the FDA’s NDC Directory to find the manufacturer. You can also ask your pharmacist directly: “Which company made this batch?” Most will tell you if you ask.
Can I ask my doctor to prevent generic switches?
Yes. Ask your doctor to write “DAW-1” (Dispense As Written) on your prescription. This legally prevents the pharmacy from substituting a different generic without your consent. This is especially important for high-risk medications. You can also request to stay on the same manufacturer by name-pharmacists can often accommodate this if the drug is available.
Is it safe to switch between different generic brands of the same drug?
For most drugs like statins or antibiotics, yes-it’s generally safe. But for drugs with a narrow therapeutic index, switching between different generic brands increases the risk of side effects or loss of effectiveness. Experts recommend staying on the same manufacturer whenever possible for these medications to avoid unpredictable changes in how your body responds.

Tim Goodfellow
December 18, 2025 AT 14:31Whoa. This post is a goddamn revelation. I never realized that my anxiety spikes after switching my Adderall generic were actually caused by the damn bead system changing. I thought I was just losing it. Turns out, the pharmacy’s playing Russian roulette with my brain. Time to start checking NDC codes like my life depends on it-because it does.
Takeysha Turnquest
December 20, 2025 AT 14:03They sell you a pill and call it the same thing
But your body knows the difference
It remembers the texture the taste the rhythm
And when it’s betrayed it screams
Jedidiah Massey
December 22, 2025 AT 10:08As a clinical pharmacist with 12 years in PBM analytics, let me break this down: FDA’s 80–125% bioequivalence window is a regulatory loophole dressed as science. For narrow TI drugs, that’s not ‘equivalent’-it’s a 45% variance in therapeutic outcome. The fact that PBMs rotate generics for rebates is a systemic betrayal. DAW-1 is your only shield. Use it. Or suffer the consequences.
Alex Curran
December 24, 2025 AT 07:06Been on warfarin for 8 years. Switched generics last year and my INR went from stable 2.3 to 5.1 in two weeks. Ended up in ER with a subdural. Never again. Always ask for the brand name. My pharmacist now keeps a sticky note on my file: NO SUBSTITUTIONS. Simple as that.
Lynsey Tyson
December 25, 2025 AT 22:38I get that generics save money. But if you’re taking something like levothyroxine and suddenly feel like you’re dragging through molasses, it’s not ‘in your head.’ I switched back to my old generic and my energy came back in 48 hours. Why should we have to be detectives just to stay healthy?
Edington Renwick
December 27, 2025 AT 02:51Of course this happens. The FDA doesn’t care about your seizures. Big Pharma owns them. They want you on the cheapest pill, even if it makes you suicidal. You think this is an accident? No. It’s profit-driven negligence. And they call it ‘healthcare.’
Allison Pannabekcer
December 27, 2025 AT 23:41If you’re on a high-risk medication, please don’t just accept the switch. Talk to your doctor. Write down your symptoms. Ask for the manufacturer. You’re not being difficult-you’re being smart. And you’re not alone. I’ve helped over 30 people track their generics and fight for stability. Your voice matters. Your body deserves consistency.
Sarah McQuillan
December 29, 2025 AT 18:34Y’all are overreacting. America’s healthcare system is the best in the world. You think other countries get this kind of access? Generics are safe. If you’re having side effects, maybe you’re just anxious. Or maybe you’re one of those people who blames pills for everything. I’ve been on generics since 2008. Still alive. Still functional. Just saying.
Aboobakar Muhammedali
December 31, 2025 AT 15:46I am from India and we use generics every day. Many people here take them without issue. But I understand for some drugs like epilepsy or thyroid, small changes matter. I think the problem is not generics itself but the lack of tracking. If we had a simple app to log which brand you took and how you felt, doctors could see patterns. Maybe that’s the real solution.
Laura Hamill
January 1, 2026 AT 04:31THIS IS A GOVERNMENT COVER-UP. The FDA and PBMs are working with Big Pharma to kill us slowly. They switch your meds to make you sick so you need MORE drugs. That’s why your anxiety spikes. That’s why your INR goes wild. They want you dependent. I found a secret database of 12,000 cases where people died after generic switches. It’s all buried. Don’t trust anyone. Check your NDC. Every. Single. Time. 🚨
Alana Koerts
January 2, 2026 AT 03:12So you’re saying the FDA’s standards are flawed? Shocking. I’m sure the 2019 BMJ study was just a fluke. And those 800 Reddit comments? Anecdotes. The real problem here is people who can’t handle change. Get over it. The system works fine for 99% of people. Stop being dramatic.
Dikshita Mehta
January 3, 2026 AT 16:18I’m a pharmacist in Kerala. We have over 100 generic manufacturers here. For most drugs, it’s fine. But for levothyroxine and phenytoin? We never switch unless the patient is stable and we document it. We also print the manufacturer name on the label in bold. It’s simple. It’s safe. Why can’t the US do this?
Kelly Mulder
January 4, 2026 AT 07:08It is imperative to underscore that the FDA’s bioequivalence parameters are statistically inadequate for medications with a narrow therapeutic index. The 45% variability allowance constitutes a gross dereliction of pharmacovigilance. Moreover, the economic incentives embedded within the PBM rebate model are not merely ethically indefensible-they are criminally negligent. The onus must shift from the patient to the regulatory apparatus. DAW-1 is not a request. It is a bioethical imperative.
Guillaume VanderEst
January 6, 2026 AT 03:38My dad had a kidney transplant. They switched his tacrolimus generic twice in six months. He almost lost the organ. We had to hire a lawyer just to get the pharmacy to stop. Now he gets his meds shipped directly from the manufacturer. It costs more. But he’s alive. That’s the only metric that matters.
Emily P
January 6, 2026 AT 16:51So… what’s the NDC code for my levothyroxine? I’ve never looked.