When you switch from a brand-name drug to a generic version, your body doesn’t just get a cheaper pill-it gets a pharmaceutical twin. The U.S. Food and Drug Administration (FDA) requires generics to match the brand-name drug in active ingredient, strength, dosage form, and how fast it enters your bloodstream. That’s not just a guideline-it’s a strict scientific standard. For most people, the switch is seamless. But for some, even tiny differences in inactive ingredients or manufacturing processes can trigger changes in how the drug works. That’s why monitoring your health after switching isn’t optional-it’s essential.
Why Some People Notice a Difference
Generics aren’t copies. They’re equivalents. The FDA mandates that the amount of active drug absorbed into your blood (measured as AUC and Cmax) must fall within 80-125% of the brand-name version. That sounds tight, but it leaves room for variation. For drugs like warfarin, levothyroxine, or lamotrigine-medications with a narrow therapeutic index-those small differences matter. A 5% change in absorption might mean your blood thinning level drops too low, your thyroid hormone dips below target, or your seizure control slips. That’s why the American Heart Association recommends extra monitoring for cardiovascular drugs after a switch.
It’s not always the drug itself. Sometimes, it’s the fillers. Generic pills may use different dyes, binders, or coatings. These don’t affect the active ingredient, but they can change how quickly the pill breaks down in your stomach. For someone with a sensitive gut, that could mean nausea, bloating, or inconsistent absorption. One patient switched from brand-name levothyroxine to a generic and noticed fatigue and weight gain. Her TSH levels jumped from 2.1 to 6.8 within three weeks. After switching back, her numbers normalized. This isn’t rare. The FDA’s 2022 report found that 12% of patients switching thyroid meds reported issues.
What to Monitor: Practical Steps
You don’t need a lab coat to monitor your health. You just need a notebook and a routine. Here’s what to track after switching:
- Symptoms: Are your headaches worse? Is your asthma tighter? Did your mood dip? Write down changes daily for at least two weeks.
- Biometrics: If you have high blood pressure, check it twice a week. If you have diabetes, test your blood sugar at least three times a week. For thyroid patients, get your TSH and free T4 tested at 4 and 8 weeks.
- Side effects: New dizziness? Unusual fatigue? Skin rash? These aren’t normal. Track when they started and how often they occur.
- Dosing consistency: Did the pill size, color, or shape change? Even if the active ingredient is the same, a different formulation can affect how your body handles it.
For chronic conditions like epilepsy, heart disease, or depression, monitor for at least 90 days. The American Academy of Family Physicians recommends a follow-up visit within 14 days of switching, especially if you’re on a high-risk medication. Don’t wait until you feel terrible-get tested early.
High-Risk Medications to Watch Closely
Not all generics are equal when it comes to switching risk. The FDA and independent studies point to a short list of drugs where patients most often report problems:
- Levothyroxine (for hypothyroidism): 12% of switchers report changes in energy, weight, or heart rate. TSH levels can swing noticeably.
- Lamotrigine (for epilepsy and bipolar disorder): 9% of users had breakthrough seizures or mood shifts after switching. The FDA recorded 62% of all reported substitution issues involved antiepileptics.
- Warfarin (blood thinner): Even small changes in absorption can lead to dangerous clots or bleeding. The American Heart Association advises INR testing at 7 and 30 days after switching.
- Bupropion (antidepressant/smoking cessation): 7% of users reported increased anxiety or reduced effectiveness. The FDA’s 2022 surveillance report flagged this as a recurring concern.
- Cyclosporine and tacrolimus (organ transplant drugs): These require constant blood level monitoring. Any switch should be done under direct medical supervision.
If you take any of these, talk to your doctor before switching. Don’t assume the pharmacy’s substitution is automatic. Ask if your prescription is marked "dispense as written"-that stops automatic generic substitution.
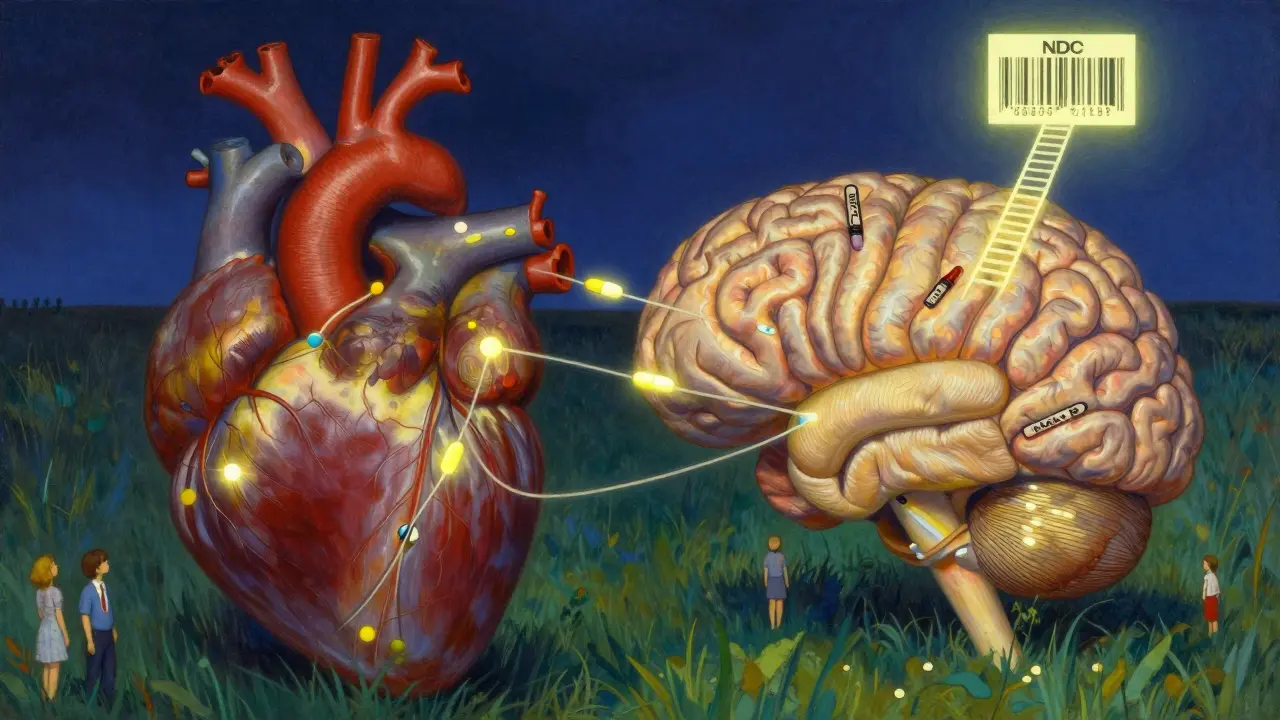
How to Verify Your Generic
Not all generics are made the same. Different manufacturers use different processes. That’s why checking the National Drug Code (NDC) on your pill bottle matters. The NDC is a unique 10-digit number that identifies the drug, manufacturer, and package size. If the NDC changes between refills, you’ve been switched to a different generic version-even if it’s the same drug name.
Use the FDA’s Orange Book (available online) to look up your medication. It lists which generics are rated as therapeutically equivalent. If your drug has an "A" rating, it’s interchangeable. If it’s "B," there may be concerns. The FDA’s 2023 guidance recommends patients check this before accepting a new generic.
What to Do If Something Feels Off
If you notice a change in how you feel, don’t ignore it. Don’t assume it’s "all in your head." Start a medication diary: write down the date you switched, the generic name, the manufacturer (look at the NDC), and your symptoms. Then:
- Call your doctor. Bring your diary. Ask for lab tests if needed.
- Ask if you can switch back to the brand-name version temporarily to see if symptoms improve.
- If your doctor agrees, request a prescription with "do not substitute" or "dispense as written."
- Report the issue to the FDA through MedWatch. You can file online at www.fda.gov/medwatch or call 1-800-FDA-1088. Include the lot number, NDC, and exact symptoms. The FDA reviews all reports and investigates serious cases within 30 days.
Most patients (over 90%) have no issues switching. But if you’re one of the few who does, your report helps others. The FDA received over 1.2 million adverse event reports in 2022, and while only 15% involved generics, each one matters.
Why Monitoring Matters More Than Ever
Generics make up 92.6% of all prescriptions in the U.S. They saved $373 billion in 2022. That’s huge. But as demand grows, so does pressure on manufacturers. In 2022, 38% of drug shortages involved generics. When supply chains get tight, companies may switch suppliers or reformulate batches quickly. That’s why checking your NDC every time you refill is no longer just smart-it’s necessary.
The FDA is stepping up surveillance. By 2025, it plans to use AI to analyze every single adverse event report related to generics within 72 hours. That’s faster than ever before. But AI can’t replace your own body’s signals. Your symptoms are the first line of defense.
Bottom Line
Switching to generics is safe for most people. But safety doesn’t mean zero risk. For certain medications and certain people, even small changes can have real effects. The key isn’t fear-it’s awareness. Track your symptoms. Know your NDC. Get tested if you’re on a high-risk drug. And if something feels off, speak up. Your health isn’t a cost-saving metric. It’s your life. And you’re the best monitor you’ve got.

Wendy Lamb
February 5, 2026 AT 08:43Just switched my levothyroxine last month. No issues. But I track my TSH every 6 weeks anyway-better safe than sorry. Keep a notebook. It’s simple, free, and saves your life.
Prajwal Manjunath Shanthappa
February 5, 2026 AT 11:57Oh, please. The FDA's '80-125%' bioequivalence window is a joke-a statistical loophole disguised as science. Real pharmacokinetics demands precision, not approximations. You're not 'equivalent' if your Cmax fluctuates like a stock market during a panic. This isn't medicine-it's pharmaceutical roulette.
Antwonette Robinson
February 5, 2026 AT 16:00So let me get this straight-you’re telling me I should spend my weekends playing detective with my pill bottle because Big Pharma wants me to save $5? Next you’ll tell me to check the NDC before I buy toilet paper.
Ed Mackey
February 6, 2026 AT 04:28i switched to generic warfarin last year and my inr went nuts. i didnt think much of it till i started bruising like a grape. called my doc, they said ‘maybe the generic’-turned out it was a different maker. switched back. fixed. dont ignore it. my bad for not checking the ndc.
Jhoantan Moreira
February 6, 2026 AT 05:47Thanks for this! 🙏 I’ve been on lamotrigine for 8 years and switched generics last winter-felt like my brain was wrapped in cotton. Got my levels checked, switched back to the original brand, and boom-clarity returned. You’re right: your body knows before your doctor does. Keep listening to it. 💙
Joseph Cooksey
February 6, 2026 AT 06:11Let’s be honest-this whole generics system is a corporate shell game dressed up as public health. The same company that makes the brand-name drug often makes the generic under a different name, same factory, same machine, just cheaper packaging. And yet, when patients report problems, they’re told it’s ‘psychosomatic’ or ‘placebo effect.’ Meanwhile, the FDA’s ‘therapeutic equivalence’ ratings are based on data from 1980s bioequivalence studies. We’re treating patients like lab rats with a spreadsheet.
And don’t get me started on the 38% drug shortages-those aren’t supply chain issues, they’re profit-driven manufacturing cuts. When your generic switch comes from a factory in Bangladesh that just got FDA approval last month, you’re not getting ‘equivalent’-you’re getting a gamble with your neurological stability.
My cousin’s on tacrolimus. Her transplant team won’t even let her touch a generic. Not because they’re elitist-they’re smart. And if you’re on anything that keeps you alive, you should be just as paranoid.
Janice Williams
February 8, 2026 AT 04:40It’s not that generics are dangerous-it’s that the medical establishment refuses to acknowledge that individuals are not statistical averages. Your body doesn’t care about FDA guidelines. It cares about how you feel. If you’re fatigued, bloated, or anxious after a switch, it’s not ‘in your head’-it’s your biochemistry screaming. The fact that 12% of thyroid patients report issues is not a rounding error. It’s a crisis of individualized care.
And yet, pharmacists still substitute automatically. Doctors still say, ‘It’s the same thing.’ And patients are left to suffer silently because no one wants to admit that biology doesn’t obey corporate cost-cutting.
Stop calling it ‘monitoring.’ Call it survival.
Meenal Khurana
February 9, 2026 AT 20:07My mom switched to generic bupropion and stopped eating. Lost 15 lbs in a month. Doctor said ‘stress.’ I said ‘check the pill.’ NDC changed. Switched back. She’s fine now. Always check the NDC.
Sherman Lee
February 11, 2026 AT 13:27Did you know the FDA gets paid by pharma companies to approve generics? 🤔 And those ‘A’ ratings? They’re not based on real-world outcomes-they’re based on 12 healthy volunteers in a lab. Real people? They’re not in the study. That’s why you’re getting weird side effects. This isn’t medicine. It’s a controlled experiment on you. And the FDA? They’re the sponsor.
Next time you get a new pill, Google the NDC. You’ll find lawsuits. You’ll find recalls. You’ll find people who died. They don’t tell you that. But now you know. 👁️🗨️