Blood Thinner & NSAID Risk Checker
This tool helps you understand the risks of combining your blood thinner with common pain relievers. Based on clinical evidence, it shows your specific risk level and emergency symptoms to watch for.
If you're on a blood thinner like warfarin, Eliquis, Xarelto, or Pradaxa, and you reach for ibuprofen or naproxen for a headache or sore knee, you're putting yourself at serious risk. This isn't a "maybe" or a "be careful" situation. It's a well-documented, life-threatening combination that sends thousands to the emergency room every year.
Why Blood Thinners and NSAIDs Don't Mix
Blood thinners don't actually make your blood thinner. They stop it from clotting the way it should. That’s the whole point - to prevent strokes, clots in the legs, or heart attacks. But when you add an NSAID like ibuprofen, naproxen, or even aspirin, you're stacking two different ways your body loses its ability to stop bleeding. NSAIDs work by blocking enzymes called COX-1 and COX-2. COX-1 is needed to make thromboxane, a chemical that helps platelets stick together and form clots. When NSAIDs shut that down, your platelets can't do their job. Meanwhile, blood thinners like warfarin or the newer DOACs (direct oral anticoagulants) interfere with clotting factors in your liver. So one drug stops platelets from working. The other stops the proteins that seal the deal. Together? Your body has almost no way to stop bleeding once it starts.The Numbers Don't Lie
A 2020 study of 200,000 patients found that taking an NSAID while on a blood thinner more than doubled your risk of internal bleeding. The risk wasn't the same for every NSAID. Naproxen increased bleeding risk by over four times. Diclofenac nearly tripled it. Even ibuprofen - the one most people think is "safe" - raised the risk by almost 80%. Where does the bleeding happen? Mostly in the gut. The risk of gastrointestinal bleeding went up by 2.24 times. But it's not just your stomach. Intracranial bleeding (bleeding in the brain) jumped by 3.22 times. That's not just a bruise - that's a stroke waiting to happen. Pulmonary and urinary bleeding also rose significantly. And nearly one in three patients on this combo ended up with severe anemia from blood loss.It's Not Just Warfarin - It's All of Them
Many people think this risk only applies to warfarin because it's older and requires regular blood tests. But the data shows otherwise. The same danger exists with Eliquis (apixaban), Xarelto (rivaroxaban), Pradaxa (dabigatran), and Savaysa (edoxaban). These newer drugs don't need INR checks, but they still thin your blood. And NSAIDs still wreck your platelets. The interaction isn't about how the blood thinner works - it's about what NSAIDs do to your body's natural stopping mechanism.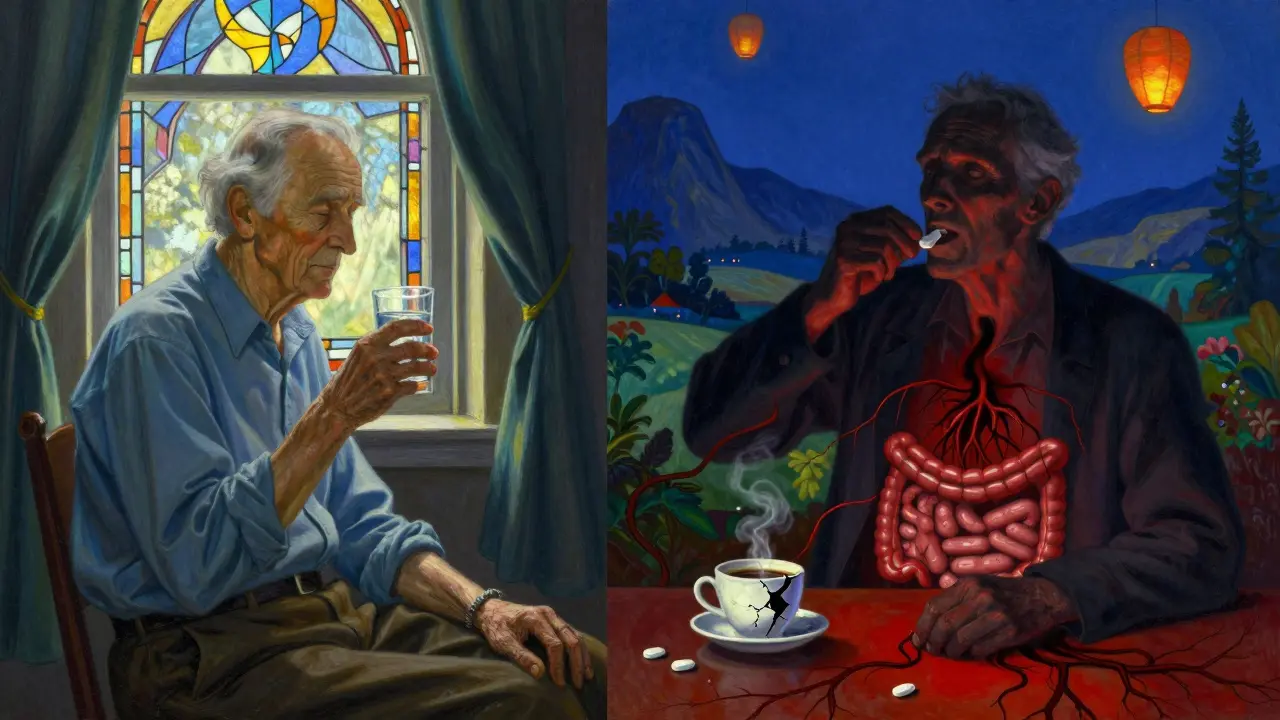
Who's at the Highest Risk?
It's not just about the drugs. Age, other meds, and health history make the danger worse. People over 65 are most at risk - not just because they're more likely to be on blood thinners for atrial fibrillation, but because they're also more likely to have arthritis, back pain, or joint issues that lead them to NSAIDs. One study found that 20-30% of people on blood thinners still take NSAIDs regularly, even after being warned. If you're also taking steroids like prednisone, or other antiplatelet drugs like clopidogrel (Plavix), your risk skyrockets. Even low-dose aspirin - often taken for heart protection - can be dangerous when combined with blood thinners. And if your INR is already on the high side (above 3.0), adding an NSAID can push you into a danger zone where bleeding becomes almost inevitable.What About "Safer" NSAIDs Like Celecoxib?
Some people hear that COX-2 inhibitors like celecoxib (Celebrex) are "gentler on the stomach" and assume they're safer with blood thinners. That's a dangerous myth. While they don't hurt the stomach lining as much, they still block platelet function just like traditional NSAIDs. A 2023 study in the Annals of Internal Medicine found that even celecoxib increased bleeding risk compared to not using any NSAID at all. It's not a loophole - it's just a slightly slower path to the same outcome.What Can You Take Instead?
Acetaminophen (Tylenol) is the go-to alternative. It doesn't affect platelets or clotting factors. But don't go overboard. Stick to 3,000 mg a day or less - higher doses can damage your liver, especially if you're older or drink alcohol. For chronic pain, physical therapy, heat wraps, or topical pain relievers like lidocaine patches or capsaicin cream can help without systemic risk. If you have arthritis or back pain, talk to your doctor about non-drug options. Weight management, low-impact exercise, and even acupuncture have shown real results. For short-term flare-ups, your doctor might prescribe a short course of corticosteroid injections - these don't interfere with clotting like NSAIDs do.What If You Already Took an NSAID?
If you accidentally took ibuprofen or naproxen while on a blood thinner, don't panic - but don't ignore it either. Watch for signs of bleeding: black or tarry stools, vomiting blood (looks like coffee grounds), unexplained bruising, nosebleeds that won't stop, headaches that feel different, or sudden weakness on one side of your body. If any of these happen, go to the ER immediately. If you're planning surgery - even a simple dental extraction - tell your doctor you're on a blood thinner. They may ask you to stop the NSAID for a few days beforehand. Ibuprofen? Stop two days before. Naproxen? Three days. Piroxicam? Ten days. These aren't guesses - they're based on how long each drug stays active in your body.Why Is This Still Happening?
Over 17 million Americans use NSAIDs every day. Twelve million are on blood thinners. That’s a huge overlap. Many people don't realize their "over-the-counter" painkiller is just as risky as a prescription drug. A 2022 study found only 43% of patients on anticoagulants knew NSAIDs were dangerous. Two-thirds thought occasional use was fine. Pharmacists sometimes miss it too. If you pick up warfarin and ibuprofen at the same pharmacy, the system might not flag it unless the pharmacist manually checks. And if you're buying OTC meds online or at a convenience store, there's no one to warn you.How to Protect Yourself
- Never take ibuprofen, naproxen, aspirin, or diclofenac without talking to your doctor first. - Keep a list of all your meds - including supplements and OTC drugs - and review it with your doctor every 6 months. - Ask your pharmacist: "Is this safe with my blood thinner?" Don't assume they'll catch it. - Use acetaminophen (Tylenol) for pain - but don't exceed 3,000 mg daily. - If you're on warfarin, get your INR checked regularly. NSAIDs can push your INR up unexpectedly. - If you're on a DOAC, don't assume you're "safe" - NSAIDs still raise bleeding risk. - Report any unusual bruising, bleeding, or fatigue to your doctor right away.This isn't about being overly cautious. It's about survival. The data is clear. The risks are real. And the consequences are often irreversible.
Can I take ibuprofen with Eliquis?
No. Taking ibuprofen with Eliquis (apixaban) significantly increases your risk of serious bleeding, including in the stomach and brain. Even occasional use can be dangerous. Acetaminophen (Tylenol) is the safer choice for pain relief while on Eliquis.
Is naproxen worse than ibuprofen with blood thinners?
Yes. Naproxen carries a much higher bleeding risk than ibuprofen when combined with blood thinners. Studies show it increases the risk of internal bleeding by over four times, compared to about 1.8 times for ibuprofen. It's one of the most dangerous NSAIDs to use with anticoagulants.
Can I take aspirin with a blood thinner?
Only under direct medical supervision. Aspirin is an NSAID and inhibits platelet function, which compounds the bleeding risk of blood thinners. In rare cases, doctors may prescribe low-dose aspirin with a blood thinner for specific heart conditions - but this is carefully monitored and not routine.
What should I do if I start bleeding while on blood thinners and NSAIDs?
Go to the emergency room immediately. Signs include black or bloody stools, vomiting blood, sudden severe headache, unexplained bruising, or bleeding that won't stop. Don't wait. This is a medical emergency.
Are there any NSAIDs that are safe with blood thinners?
No NSAID is truly safe with blood thinners. Even COX-2 inhibitors like celecoxib still raise bleeding risk. The only safe option is to avoid all NSAIDs and use acetaminophen or non-drug therapies for pain instead.
How long should I stop NSAIDs before surgery if I'm on a blood thinner?
Stop ibuprofen at least 2 days before surgery, naproxen 2-3 days, and piroxicam 10 days. Always confirm with your doctor - the timing depends on your specific blood thinner, health, and type of procedure.
Why do doctors still prescribe NSAIDs to people on blood thinners?
They shouldn't - but sometimes they do out of habit, lack of awareness, or because the patient is in severe pain and no alternatives were discussed. Many patients also self-medicate with OTC NSAIDs without telling their doctor. This is why patient education is critical.
Can I use topical NSAIDs like diclofenac gel while on blood thinners?
Topical NSAIDs are absorbed in much smaller amounts, so the risk is lower than pills. But they're not risk-free, especially if you're using large amounts, applying them to broken skin, or using them long-term. Talk to your doctor before using them - acetaminophen or physical therapy are still safer first choices.

saurabh singh
January 5, 2026 AT 21:57Man, I just learned this the hard way last year. My dad was on Xarelto and took ibuprofen for his knee pain for weeks. Ended up in the ER with a GI bleed. They didn’t even flag it at the pharmacy. If you’re on a blood thinner, treat OTC painkillers like grenades. Tylenol is your only friend now.
John Wilmerding
January 6, 2026 AT 12:12It is imperative to underscore that the pharmacodynamic interaction between nonsteroidal anti-inflammatory agents and anticoagulants constitutes a Class I contraindication per the American College of Cardiology guidelines. The combined inhibition of platelet aggregation and coagulation cascade significantly elevates the risk of clinically significant hemorrhage, particularly in the gastrointestinal and central nervous systems. Acetaminophen remains the sole recommended analgesic in this population, with dosing not exceeding 3,000 mg daily to mitigate hepatotoxicity risk.
Peyton Feuer
January 7, 2026 AT 05:11so like… i thought celecoxib was safe? turns out it’s just a fancy naproxen with a better ad? wow. thanks for the heads up. i’ve been taking it for my back and just assumed it was ‘gentle’. my bad. going to switch to tylenol now.
Siobhan Goggin
January 8, 2026 AT 22:54My uncle had a stroke after taking naproxen with warfarin. He didn’t even realize it was dangerous. People need to stop treating OTC meds like harmless candy. This post should be mandatory reading for anyone over 50.
Vikram Sujay
January 9, 2026 AT 00:56One cannot help but reflect on the paradox of modern medicine: we possess the tools to prevent catastrophic cardiovascular events, yet we persist in the casual administration of substances that undermine these very protections. The cultural normalization of NSAIDs as benign, over-the-counter remedies reflects a broader epistemological failure - the assumption that accessibility equates to safety. The data is unequivocal. The human cost is not abstract. It is a father, a mother, a neighbor - bleeding internally, unaware, until it is too late.
Jay Tejada
January 10, 2026 AT 13:34lol so basically the only thing you can take for pain is tylenol… which kills your liver if you take it too much… and if you’re old and on blood thinners you’re just supposed to suffer? nice. thanks for the life hack, doc.
Shanna Sung
January 11, 2026 AT 17:38They’re hiding the truth. NSAIDs are fine. It’s the blood thinners that are the real problem. Big Pharma wants you scared so you’ll keep buying their $500 pills. The FDA is in the pocket of the drug companies. I took ibuprofen with Eliquis for 3 years. No problems. Until they told me to stop. Then I got worse pain. Coincidence? I think not.
Allen Ye
January 12, 2026 AT 23:06Let’s take a step back and look at the systemic failure here. We have a population aging rapidly, burdened by chronic pain, and yet the medical infrastructure is still stuck in a 1990s mindset where doctors assume patients read pamphlets and pharmacists are omniscient. We’re not just talking about individual negligence - we’re talking about a public health blind spot. The fact that 57% of patients don’t know NSAIDs are dangerous isn’t a failure of education - it’s a failure of design. Why isn’t every OTC painkiller package printed with a blood thinner warning in bold red? Why isn’t there a mandatory pop-up when you buy ibuprofen at CVS if you’ve picked up warfarin in the last 6 months? We’ve built a system that assumes people are doctors, when we should be building systems that assume people are human - distracted, tired, in pain, and trusting.
mark etang
January 12, 2026 AT 23:33Thank you for this comprehensive and evidence-based overview. This information is critical for patient safety and should be disseminated through all clinical channels. Healthcare providers must prioritize patient education and implement standardized screening protocols for NSAID use in anticoagulated populations. Adherence to these guidelines can significantly reduce preventable hemorrhagic events.