Allergic Conjunctivitis Treatment Advisor
Get personalized treatment recommendations
Based on your symptoms and triggers, we'll suggest the most appropriate treatment options.
Treatment Options Overview
| Medication Type | Best For | Onset Time | |
|---|---|---|---|
| Antihistamine eye drops | Mild to moderate itching | 5-10 minutes | |
| Mast cell stabilizers | Preventive control (especially seasonal) | 3-7 days | |
| Oral antihistamines | Combined nasal and eye symptoms | 30-60 minutes | |
| Artificial tears | Mild cases and dry eye component | Immediate | |
| Corticosteroids | Severe cases (short-term only) | Within minutes | High risk with long-term use |
How to Use This Tool
Select your symptoms and triggers to receive personalized recommendations.
This tool is for informational purposes only and not medical advice. Always consult an eye doctor for diagnosis and treatment.
When your eyes feel itchy, red, and watery, it’s easy to chalk it up to a stray speck of dust. But if the irritation keeps coming back every spring or after a pet cuddle, you might be dealing with allergic conjunctivitis. In this guide we break down what triggers it, how to spot it, and what you can do to get relief fast.
What Is Allergic Conjunctivitis?
Allergic conjunctivitis is a type of eye inflammation that occurs when the conjunctiva - the thin, clear tissue covering the white of the eye and the inside of the eyelids - reacts to allergens. It’s not an infection, so antibiotics won’t help; instead the immune system releases chemicals that cause redness, itching, and a watery discharge.
Why Does It Happen? Common Triggers
Allergies are essentially an over‑reaction of your immune system. When you encounter an allergen, certain cells called mast cells release a chemical messenger known as histamine. Histamine widens blood vessels and makes nerves fire, which is why you feel that classic itch.
- Pollen: Tree, grass, and weed pollen are the top culprits during spring, summer, and fall.
- Animal dander: Proteins from cat or dog skin flakes can linger on clothing and furniture.
- Dust mites: Tiny insects that love warm, humid environments like bedrooms.
- molds: Spores become airborne in damp basements or after heavy rain.
- Chemical irritants: Smoke, perfume, or cleaning agents can aggravate an already sensitive eye.
In many cases, the trigger is seasonal, which is why you’ll hear people call it “hay‑fever eye.”
Spotting the Symptoms
The signs of allergic conjunctivitis are pretty consistent, but they can vary in intensity:
- Intense itching - the urge to rub your eyes is almost irresistible.
- Redness, especially around the inner eyelid.
- Watery discharge that looks clear, not yellow or green.
- Slight swelling of the eyelids or conjunctiva (known as chemosis).
- Sensitivity to light (photophobia) in more severe cases.
If you notice thick, colored discharge or severe pain, it could be a bacterial infection or another eye condition, and you should see a professional right away.
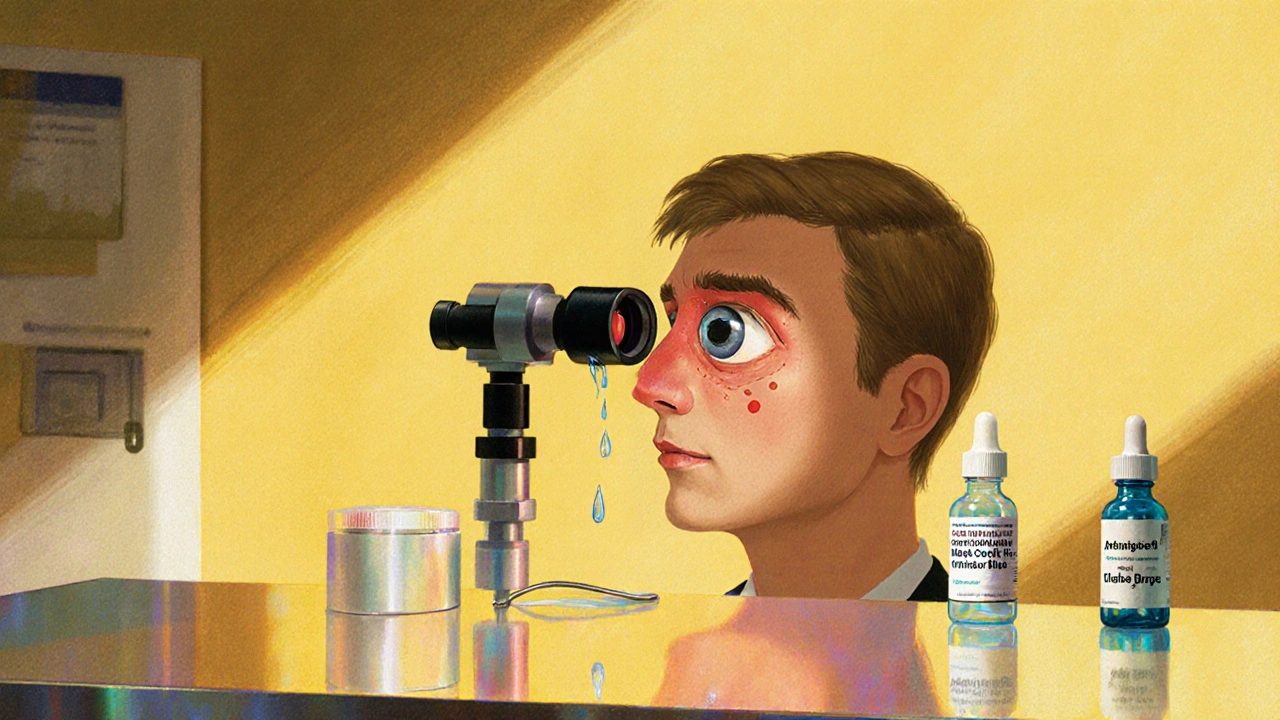
How Doctors Confirm the Diagnosis
Most eye doctors (ophthalmologists or optometrists) can diagnose allergic conjunctivitis just by looking at your eyes with a slit‑lamp. They’ll ask about:
- Recent exposure to known allergens (pollen count, pet contact, etc.).
- Family history of allergies or asthma.
- Any over‑the‑counter eye drops you’ve tried.
In rare cases, they might perform a conjunctival scrap test to check for specific allergen antibodies.
Treatment Options - What Works Best?
Because the problem stems from histamine release, most treatments target that pathway. Below is a quick comparison of the main options you’ll encounter.
| Medication Type | How It Works | Typical Onset | Best For | Common Side Effects |
|---|---|---|---|---|
| Antihistamine eye drops | Blocks histamine receptors in the eye | 5‑10 minutes | Quick relief of itching and redness | Mild stinging, temporary blurred vision |
| Mast cell stabilizer drops | Prevents mast cells from releasing histamine | Several days of regular use | Preventive control, especially for seasonal allergies | Rare irritation, slight burning |
| Oral antihistamines | Systemic blockage of histamine receptors | 30‑60 minutes | When eye drops alone aren’t enough or you have nasal symptoms | Dry mouth, drowsiness (non‑sedating versions available) |
| Artificial tears | Lubricates the eye, dilutes irritants | Immediate | Dry‑eye component of allergy, mild cases | Usually none, may cause temporary blur |
| Corticosteroid eye drops | Strong anti‑inflammatory action | Within minutes | Severe or refractory cases (short‑term use only) | Increased eye pressure, cataract risk with long use |
For most people, a combination of antihistamine eye drops and a mast cell stabilizer works well. Use the stabilizer daily before the allergy season starts, and keep the antihistamine on hand for flare‑ups.
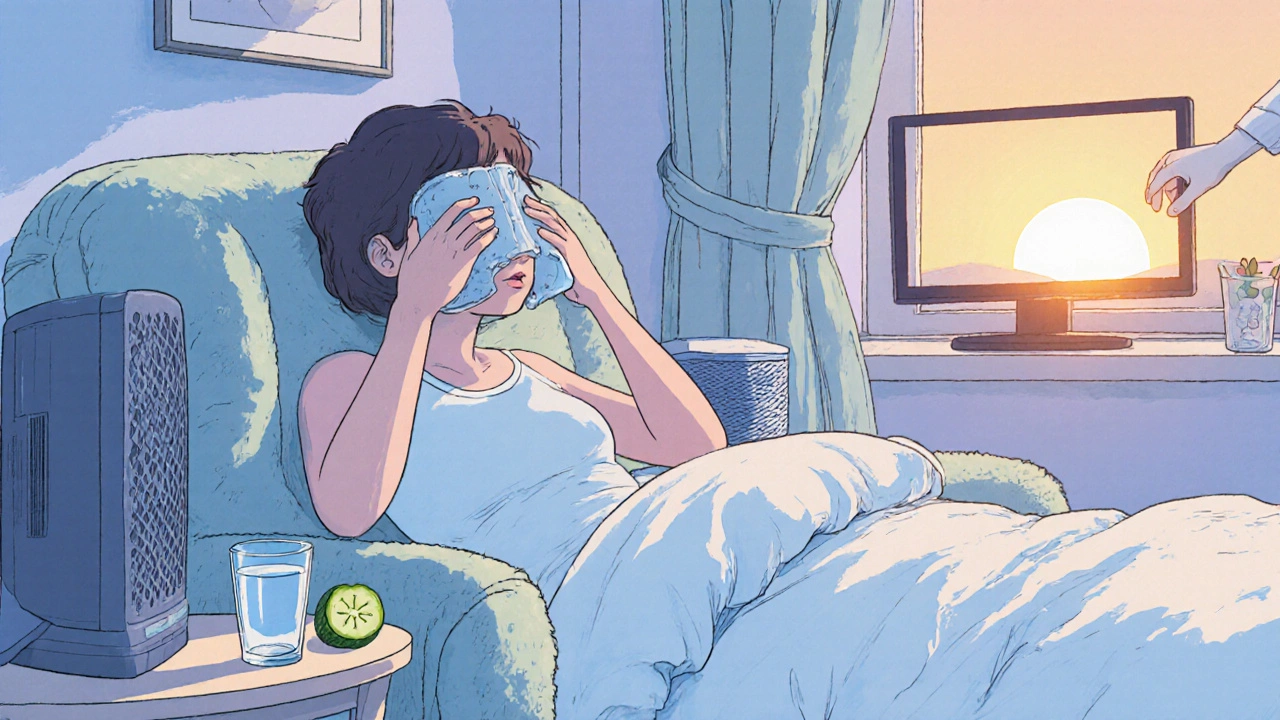
Do-It-Yourself Relief Tips
While medication does the heavy lifting, everyday habits can cut down on exposure and soothe irritation:
- Cold compress: Place a clean, chilled washcloth over closed eyes for 5‑10 minutes to reduce swelling.
- Stay hydrated: Drinking water helps thin the mucus layer on the eye surface.
- Limit screen time: Staring at a screen dries out the eyes, making itching worse.
- Change bedding weekly: Dust mites love the warm, moist environment of sheets.
- Use air filters: HEPA filters trap pollen and pet dander indoors.
Remember not to rub your eyes - it can damage the delicate lining and push allergens deeper.
When to Call an Eye Professional
Most allergic conjunctivitis cases improve with OTC drops and lifestyle tweaks. Seek professional care if you notice any of these red flags:
- Eye pain that’s sharp or persistent.
- Vision changes - blurriness that won’t clear up.
- Thick, colored discharge (yellow, green, or white).
- Symptoms lasting longer than two weeks despite treatment.
- History of severe eye allergies or previous steroid use.
The doctor can rule out infections, prescribe short‑term steroids if needed, and advise on long‑term allergy management plans.
Quick Reference Checklist
- Identify common triggers (pollen, dander, dust).
- Track symptom patterns - keep a simple diary.
- Start preventive mast cell stabilizer drops 1‑2 weeks before season.
- Keep antihistamine drops handy for instant relief.
- Use artificial tears throughout the day to stay lubricated.
- Apply cold compresses for swelling.
- Upgrade home air filtration and clean bedding regularly.
- Consult your eye doctor if pain, vision loss, or long‑lasting symptoms appear.
Frequently Asked Questions
Can allergies cause permanent eye damage?
Rarely. Chronic rubbing or untreated severe inflammation can lead to corneal scratches, but prompt treatment usually prevents lasting harm.
Are there natural remedies that work?
Cold cucumber slices, chamomile tea eye rinses, and omega‑3 rich foods can soothe symptoms, but they’re best used alongside proven medications.
What’s the difference between allergic and viral conjunctivitis?
Allergic conjunctivitis produces clear watery discharge and intense itching, while viral forms often cause a thicker, yellowish discharge and may be contagious.
Can I wear contact lenses during an allergy flare?
It’s safer to switch to glasses until symptoms subside. Contacts can trap allergens and worsen irritation.
How long does treatment usually take to work?
Antihistamine drops start relieving itching within minutes; mast cell stabilizers need a few days of consistent use to build protection.
Allergic conjunctivitis can be a nuisance, but with the right mix of preventive drops, quick‑acting antihistamines, and simple lifestyle tweaks, you can keep your eyes clear and comfortable all year round.

Kirsten Youtsey
October 20, 2025 AT 20:45In the vast tapestry of ocular therapeutics, one observes an unmistakable trend toward the consolidation of pharmaceutical conglomerates under the guise of benevolent innovation.
The very formulations touted as miracle drops are, upon closer scrutiny, the product of a relentless quest for market dominance.
Consider, for instance, the ubiquitous antihistamine eye drops that flood our shelves each spring; their active ingredient is seldom disclosed beyond a generic label.
Such opacity invites speculation that ancillary compounds, perhaps designed to augment consumer dependence, remain hidden from the discerning eye.
A parallel can be drawn to the alleged "natural" alternatives, which are frequently shepherded by the same corporate entities that engineer synthetic analogues.
It is not merely a coincidence that the same brands dominate both the over‑the‑counter aisles and the premium boutique pharmacies.
The regulatory apparatus, ostensibly the guardian of public health, appears at times to be complicit, granting expedited approvals to formulations that have undergone scant longitudinal study.
One must ask whether the expedited pathways are justified by genuine therapeutic necessity or by an undisclosed alliance between industry lobbyists and policy makers.
Historical precedent, dating back to the mid‑twentieth century, illustrates the perils of entrusting ocular health to entities whose primary motive is profit.
The infamous case of the preservative‑laden drops that precipitated chronic keratoconjunctivitis serves as a cautionary tale.
Yet today, similar preservative profiles persist, cloaked in modern marketing slogans that promise “rapid relief” and “clinically proven efficacy.”
Such rhetoric masks the underlying pharmacodynamics, which often rely on transient vasoconstriction rather than true immunomodulation.
Patients, eager for respite, inadvertently become participants in an inadvertent, long‑term exposure experiment.
While the immediate symptom relief is undeniable, the potential cumulative impact on the ocular surface remains insufficiently documented.
Thus, a judicious approach-favoring preservative‑free formulations, rigorous environmental controls, and a skeptical appraisal of corporate claims-is advisable.
In sum, the discerning eye should remain vigilant, lest the allure of convenience eclipse the imperative of ocular integrity.
Matthew Hall
October 24, 2025 AT 08:05Man, the moment pollen hits, it feels like the government’s secret fog machines are back in action, turning our eyes into assault zones.
Those cheap eye drops they push on the shelves are probably just diluted mist with a dash of mind‑control serum, if you ask me.
I swear, every time I open a new bottle, the label whispers a warning that my eyes will never be the same again.
All I want is a clear view of the world without feeling like I’m starring in a low‑budget horror flick.
So I keep my windows shut, my curtains drawn, and hope the next wave of “natural” sprays is just a myth.
Deja Scott
October 27, 2025 AT 18:25Allergic conjunctivitis, while common, reflects the broader interplay between environment and ocular health across cultures.
In many societies, traditional eye‑soothing practices coexist with modern pharmacology, offering a holistic perspective.
Recognizing these varied approaches can enrich our understanding of effective management.
Natalie Morgan
October 31, 2025 AT 05:45Stay ahead of the season by tracking pollen counts daily.
A simple habit of rinsing eyes with cool water each morning can cut down irritation dramatically.
Combine that with preservative‑free drops and you’ll feel the difference within minutes.
Keep the momentum and your eyes will thank you.
Mahesh Upadhyay
November 3, 2025 AT 17:05Your eyes deserve more than disposable drops marketed for profit.
Choose products that respect the delicate ocular barrier.
Avoid preservatives that masquerade as harmless.
Educate yourself on the ingredients, not just the brand.
Only then can you truly safeguard your vision.
Rajesh Myadam
November 7, 2025 AT 04:25I understand how frustrating it can be when the season changes and your eyes start burning.
Many of us have found relief by keeping a small bottle of artificial tears at the desk.
It helps to rinse away pollen before it settles on the eye surface.
Couple that with a nightly cold compress and you’ll notice less swelling.
If symptoms persist, a quick visit to the optometrist can pinpoint if a stronger prescription is needed.
laura wood
November 10, 2025 AT 15:45Your deep dive into the industry’s hidden motives really opened my eyes to the need for vigilance.
I’ll definitely start checking for preservative‑free options after reading your analysis.
Kate McKay
November 14, 2025 AT 03:05You nailed the ethical angle-our eyes are not commodities.
Encourage others to read labels and demand transparency.
That small step can spark a larger movement toward responsible eye care.
Demetri Huyler
November 17, 2025 AT 14:25While your theatrical warnings are entertaining, the reality is far less conspiratorial.
The majority of ocular drops undergo rigorous testing before hitting the market.
Nevertheless, a degree of consumer skepticism is healthy, especially regarding preservative content.
A balanced view serves both the informed elite and the everyday user.
Israel Emory
November 21, 2025 AT 01:45Indeed, the cultural nuances, ranging from Ayurvedic eye washes to Scandinavian hygge‑inspired relaxation, enrich our collective knowledge, and they deserve recognition.
Moreover, each tradition, whether rooted in ancient herbal lore or modern clinical practice, contributes a unique perspective, fostering a holistic approach to ocular health.
Thus, integrating these diverse methods, while maintaining rigorous scientific standards, can only benefit the global community.
Sebastian Green
November 24, 2025 AT 13:05Energetic daily rinses truly make a noticeable difference.
Wesley Humble
November 28, 2025 AT 00:25Your pragmatic suggestions, though well‑intentioned, overlook the empirical data that distinguishes efficacious formulations from mere placebos.
A comprehensive meta‑analysis reveals that preservative‑free agents consistently outperform their preserved counterparts in reducing ocular hyperemia.
Therefore, the recommendation to merely ‘visit the optometrist’ is insufficient without specifying the necessity for a targeted antihistamine regimen.
Consider this an invitation to elevate the discourse, 😊 and perhaps to adopt evidence‑based protocols in your personal regimen.