Every year, thousands of people end up in emergency rooms not because of an accident or a bad diet, but because they took a pill and had a drink. It sounds simple-take your medicine, enjoy a beer or glass of wine. But when alcohol meets prescription drugs, the result isn’t just a hangover. It can be a stopped breath, a collapsed liver, or a fatal fall. And most people have no idea they’re playing Russian roulette with their health.
Why Alcohol and Prescription Drugs Don’t Mix
Alcohol doesn’t just sit there while your medication does its job. It gets in the way-sometimes quietly, sometimes violently. The body treats both alcohol and many medications the same way: they’re processed in the liver by the same set of enzymes. When alcohol is present, it can either slow down or speed up how fast your body breaks down the drug. That means your medicine might not work at all-or it might build up to toxic levels. Take warfarin, a blood thinner. If you drink even a couple of drinks while taking it, your blood can become dangerously thin. A 2018 study showed alcohol can increase warfarin levels by up to 35%, raising the risk of internal bleeding. On the flip side, if you drink regularly, your liver starts working overtime to break down alcohol. That makes it process warfarin too fast, leaving you unprotected from clots. Either way, you’re at risk.The Deadliest Combos: Opioids and Benzodiazepines
Some interactions aren’t just risky-they’re deadly. The worst offenders are opioids like oxycodone and hydrocodone, and benzodiazepines like Xanax, Valium, and Ativan. Both types of drugs slow down your central nervous system. So does alcohol. When you combine them, the effect isn’t added-it’s multiplied. Research from the CDC shows that mixing alcohol with opioids increases the risk of fatal respiratory depression by six times. Even one drink with a standard opioid dose can double your chance of dying in a car crash. In 2022 alone, alcohol-opioid interactions were linked to 2,318 overdose deaths in the U.S. That’s not a statistic-it’s 2,318 families who lost someone who thought one beer wouldn’t hurt. Benzodiazepines are no better. Combine them with alcohol and sedation spikes by 400%. People don’t just feel sleepy-they pass out. In older adults, this leads to falls. A 2017 study found that seniors who drank while taking benzodiazepines were 50% more likely to fall and break a hip. Many never walk again.Other Dangerous Pairings You Might Not Expect
It’s not just the heavy hitters. Even common medications can turn dangerous with alcohol. Acetaminophen (Tylenol) is one of the most widely used painkillers. But if you drink regularly-just a glass or two a day-it can cause acute liver failure. The FDA estimates that 1 in 200 regular drinkers who take acetaminophen will suffer liver damage severe enough to need a transplant. It doesn’t take much: three drinks a day with a standard dose of Tylenol can trigger it. NSAIDs like ibuprofen or naproxen are often taken for arthritis or back pain. But with alcohol, they can cause stomach bleeding. A study of 200,000 patients showed heavy drinkers who took NSAIDs had a 300% higher risk of gastrointestinal bleeding. That’s three times more likely than someone who just took the pill. Even antidepressants like SSRIs (Prozac, Zoloft) aren’t safe. While they don’t cause fatal interactions, they make you drowsy. A 2021 study found that 35% of people over 65 who drank even one drink a day while on SSRIs felt so sleepy they nearly fell over. For seniors, that’s a fall waiting to happen.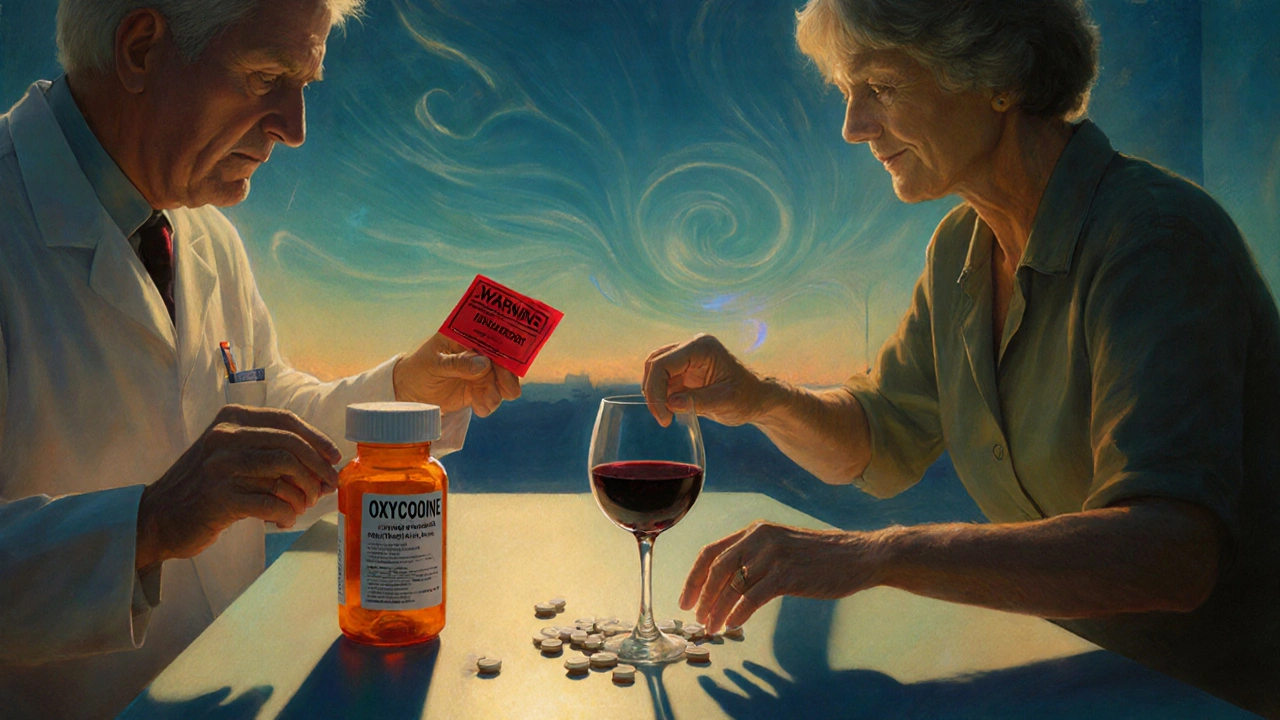
Who’s Most at Risk?
It’s not just about what you take-it’s about who you are. Older adults are hit hardest. As we age, our livers slow down. Alcohol stays in the system longer. Medications build up faster. Adults over 65 experience three times more severe interactions than younger people. And yet, 42% of U.S. seniors take both alcohol and a medication with known interaction risks. Women are more vulnerable too. Because of lower body water content and slower alcohol metabolism, the same amount of alcohol affects them more. A drink that’s safe for a man might push a woman into danger. People with liver disease are in even greater danger. If your liver is already damaged, adding alcohol to acetaminophen or even some antibiotics like isoniazid can push it into failure. Their risk of toxicity is five times higher.Why Doctors Don’t Always Warn You
You’d think your doctor or pharmacist would tell you. But they often don’t. A review of 12,450 patient reviews on Healthgrades found that 68% of people prescribed benzodiazepines were never warned about alcohol. One patient wrote: “My doctor never mentioned I shouldn’t drink on Xanax.” Another said: “I had two beers after my surgery and couldn’t breathe for 20 minutes.” Why? Because warning labels are inconsistent. Only 38% of benzodiazepine prescriptions include a clear alcohol warning, according to a 2022 FDA audit. Many doctors assume patients know. Many patients assume it’s fine. But pharmacists often catch what doctors miss. One Google Review from a pharmacy in Sydney reads: “My pharmacist refused to fill my lorazepam prescription when I admitted I drank every night. He said, ‘I’ve seen too many people die from this.’ He probably saved my life.”
What You Can Do Right Now
You don’t need a medical degree to protect yourself. Just follow these steps:- Check the label. Look for the words “Avoid alcohol” or “May cause drowsiness.” If it’s there, take it seriously.
- Ask your pharmacist. They’re trained to spot interactions. Ask: “Is it safe to drink while taking this?” Don’t be embarrassed. It’s their job.
- Use the NIAAA Alcohol Medication Check app. It lets you scan your prescription and instantly tells you if alcohol is risky with it. It covers over 2,300 medications.
- Use visual risk tools. Some pharmacies now use red, yellow, and green codes on labels. Red = don’t drink. Yellow = talk to your doctor. Green = low risk. Ask for it.
The Bigger Picture: Why This Keeps Happening
This isn’t just about individual choices. It’s a system failure. The global market for drug interaction software is growing fast-projected to hit $2.8 billion by 2030. Hospitals like the VA now use AI tools that flag alcohol-drug risks in real time. In facilities that use these systems, adverse events dropped by 28%. But in private clinics? Not so much. Only 32% of private practices screen for alcohol use when prescribing. And in Australia, where alcohol is part of social life, awareness is even lower. New laws are starting to change that. The 2022 Alcohol-Drug Interaction Labeling Act in the U.S. now requires clear warnings on high-risk prescriptions. In Australia, similar guidelines are being drafted. But until every doctor, pharmacist, and patient understands the danger, people will keep dying quietly.Final Thought: One Drink Isn’t Just One Drink
You might think, “I only have one glass of wine.” Or, “I only drink on weekends.” But with some medications, there’s no safe amount. One drink with an opioid can kill. One drink with warfarin can bleed you out. One drink with Tylenol can destroy your liver over time. The truth is, alcohol isn’t just a social drink. For millions of people on prescription meds, it’s a silent killer. And the most dangerous part? Most of these deaths are completely preventable. If you’re on any prescription medication, ask yourself: Have I ever been told not to drink with it? If the answer is no-ask now. Don’t wait for a hospital visit. Don’t wait for a near-death experience. Your life might depend on it.Can I have one drink with my prescription medication?
It depends on the medication. For opioids, benzodiazepines, or blood thinners like warfarin, even one drink can be dangerous. For others, like some antibiotics, it may be low risk-but never assume. Always check with your pharmacist. There’s no universal rule: one drink with one drug might be safe, but with another, it could be fatal.
Do over-the-counter meds like Tylenol interact with alcohol?
Yes, and it’s more dangerous than most people realize. Regular alcohol use with acetaminophen (Tylenol) can cause acute liver failure. The FDA says 1 in 200 regular drinkers who take it daily will suffer serious liver damage. This risk increases dramatically if you drink more than three drinks a day or have liver disease.
Why don’t doctors always warn patients about alcohol interactions?
Many doctors assume patients know. Others don’t have time during short appointments. Warning labels on prescriptions are inconsistent-only 38% of benzodiazepine prescriptions include alcohol warnings. A 2023 study found 43% of primary care physicians couldn’t correctly identify all high-risk drug classes. It’s a gap in the system, not just patient ignorance.
Is it safe to drink alcohol while taking antidepressants?
It’s not recommended. While SSRIs like Zoloft or Prozac don’t cause fatal interactions, alcohol can double drowsiness and dizziness. For people over 65, this increases fall risk significantly. Studies show 35% of older adults on SSRIs who drink even one drink a day report extreme sleepiness. The risk isn’t death-it’s injury from falling.
What should I do if I accidentally mixed alcohol with my medication?
If you feel unusually drowsy, confused, have trouble breathing, or experience chest pain or vomiting, seek medical help immediately. Don’t wait. Call emergency services or go to the nearest hospital. Even if you feel fine, it’s wise to contact your pharmacist or doctor. Some reactions take hours to show up.
Are there apps or tools to check for alcohol-drug interactions?
Yes. The NIAAA’s free ‘Alcohol Medication Check’ app lets you scan or search your prescription to see if alcohol is risky. GoodRx and Medscape also offer interaction checkers. Pharmacies in Australia and the U.S. are starting to use visual risk tools (red/yellow/green) on labels. Ask your pharmacist if they use them.

Brian Bell
November 15, 2025 AT 18:57Ashley Durance
November 17, 2025 AT 02:01Ryan Anderson
November 17, 2025 AT 22:42gent wood
November 19, 2025 AT 19:20Hrudananda Rath
November 20, 2025 AT 13:16Kevin Wagner
November 22, 2025 AT 05:52Dilip Patel
November 23, 2025 AT 18:19Eleanora Keene
November 24, 2025 AT 17:20Scott Saleska
November 26, 2025 AT 11:12Don Ablett
November 27, 2025 AT 14:53Nathan Hsu
November 28, 2025 AT 04:04Brian Bell
November 29, 2025 AT 05:55