Alcohol & Medication Interaction Checker
Select your medication and age group to see interaction risks.
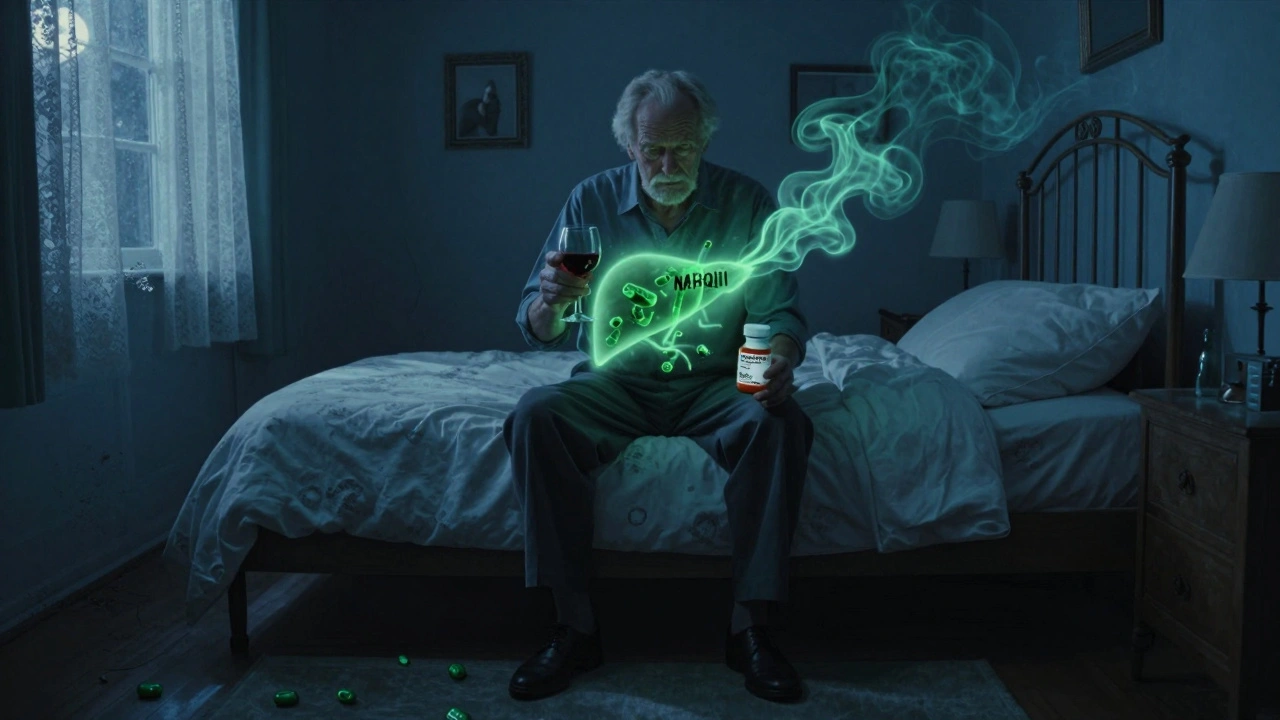
More than 40% of adults in the U.S. took a medication last year that could react dangerously with alcohol. That’s not a small number-it’s a silent risk many people don’t even realize they’re taking. Whether it’s a painkiller after a long day, a sleep aid, or even a common cold medicine, mixing alcohol with medications isn’t just a bad idea-it can be deadly.
Why Alcohol and Medications Don’t Mix
Alcohol doesn’t just sit there quietly in your body. It’s processed by the liver, same as most medications. When both are present, they compete for attention. This slows down how fast your body breaks down the drug, or sometimes speeds it up in a dangerous way. The result? Too much of the drug builds up in your system, or not enough gets absorbed to work properly. But it’s not just about metabolism. Alcohol also affects your brain and nervous system. Many medications do the same. When they team up, the effects multiply. Think of it like pressing the gas and brake at the same time-your body doesn’t know what to do, and things can go wrong fast.Deadly Combinations: Opioids, Benzodiazepines, and Alcohol
The most dangerous mix is alcohol with opioids (like oxycodone, hydrocodone, or methadone) or benzodiazepines (like Xanax, Valium, or Klonopin). Both alcohol and these drugs slow down your breathing. Together, they can shut it down completely. The FDA removed a popular extended-release opioid, Palladone, from the market after studies showed alcohol could cause a sudden flood of the drug into the bloodstream-leading to overdose and death. A 2019 study in the Journal of Substance Abuse Treatment found that mixing alcohol with benzodiazepines increases the risk of overdose by 24 times. In 2020, the CDC reported that 20% of opioid-related deaths also involved alcohol. These aren’t rare accidents. They’re predictable outcomes of a simple, common mistake.Acetaminophen: The Silent Liver Killer
You probably have acetaminophen (Tylenol) in your cabinet. It’s in hundreds of over-the-counter cold and pain medicines. But if you drink alcohol-even just one or two drinks a day-and take it regularly, you’re putting your liver at serious risk. The liver breaks down acetaminophen into a toxic chemical called NAPQI. Normally, your body neutralizes it with antioxidants. But alcohol depletes those antioxidants. Without them, NAPQI builds up and starts destroying liver cells. The FDA says acetaminophen overdose, often triggered by alcohol use, causes 56,000 emergency room visits and nearly 500 deaths every year in the U.S. alone. You don’t need to take a whole bottle. Just a few extra doses over a few days, with a glass of wine or beer, can be enough.NSAIDs and Your Stomach
Ibuprofen (Advil), naproxen (Aleve), and aspirin are common pain relievers. They’re fine on their own. But add alcohol, and you’re increasing your chance of stomach bleeding by 3 to 5 times. The alcohol irritates the stomach lining. The NSAID blocks protective chemicals. Together, they create a perfect storm for ulcers and internal bleeding. This isn’t just a concern for heavy drinkers. Even occasional use-say, a beer after taking ibuprofen for a headache-can be risky, especially if you’re older or have a history of stomach issues.
Antibiotics, Antidepressants, and Other Surprises
Some antibiotics, like metronidazole (Flagyl), cause a violent reaction when mixed with alcohol. You’ll get nausea, vomiting, flushing, rapid heartbeat, and even chest pain. This isn’t just discomfort-it’s a medical emergency. The Illinois Poison Center recommends waiting at least 72 hours after your last dose before drinking. Even SSRIs like Prozac or Zoloft aren’t safe. Alcohol can make depression worse, reduce the medication’s effectiveness, and increase dizziness or drowsiness. It doesn’t cancel out the drug-it just makes you feel worse while doing nothing to help your mood. Blood pressure meds? Alcohol can cause your blood pressure to drop suddenly, especially when standing up. That’s a fall risk. For older adults, that can mean a broken hip or worse.Who’s Most at Risk?
Older adults are the most vulnerable. By age 65, most people are taking multiple medications-on average, 14 prescriptions a year. Their bodies process alcohol slower, and their liver function declines. The Beers Criteria, used by doctors to flag risky drugs for seniors, lists 30 medications that shouldn’t be mixed with alcohol, including common sleep aids, muscle relaxers, and first-gen antihistamines like Benadryl. Women are also at higher risk. Because of differences in body composition and metabolism, women reach higher blood alcohol levels than men after drinking the same amount. That means even small amounts of alcohol can have stronger effects when combined with medication. Veterans and people with mental health conditions face even greater risks. The VA found that 30% of veteran suicides involved alcohol and prescription drugs. People with both depression and alcohol use disorders are 3.5 times more likely to experience harmful interactions.What You Can Do
The best advice is simple: don’t drink alcohol if you’re taking any medication unless your doctor says it’s safe. But if you’re unsure, here’s what to do:- Read the label. The FDA requires warning labels on about 100 prescription drugs and 700 over-the-counter medicines that interact with alcohol.
- Ask your pharmacist. They see every medication you pick up. They’re trained to spot dangerous combinations.
- Check your meds online. Use trusted sources like Healthdirect.gov.au or the NIAAA’s online tool to look up your specific drug.
- Keep a list. Write down every pill, supplement, and herbal remedy you take. Bring it to every doctor visit.
- Wait. If you’re on metronidazole, wait 72 hours after your last dose. For some antidepressants, even a few days without alcohol helps.

What About ‘Just One Drink’?
Many people think, “I’m not a heavy drinker. One glass of wine won’t hurt.” But that’s exactly how people get hurt. A single drink can be enough to trigger a reaction with certain medications. There’s no safe threshold for mixing alcohol and drugs like opioids, benzodiazepines, or metronidazole. For others, like metformin or blood pressure meds, even one drink can be risky if you’re older or have other health issues. The idea of “moderation” doesn’t apply here. With some medications, there is no safe amount of alcohol.Doctors Aren’t Always Talking About It
A 2022 study in JAMA Internal Medicine found that only 35% of primary care doctors routinely ask patients about alcohol use when prescribing medications. That means most people aren’t getting the warning they need. That’s why you have to be your own advocate. Don’t wait for your doctor to bring it up. Ask: “Is it safe to drink alcohol with this medication?” If they’re unsure, ask for a referral to a pharmacist. Pharmacists are medication experts-and they’re often more up to date on interactions than doctors.The Future: Better Warnings, Better Tools
New technology is starting to help. Electronic health records now have alerts that block doctors from prescribing high-risk drugs to patients with known alcohol use. The FDA now requires new extended-release opioids to be tested with alcohol before approval. Research is also moving toward personalized medicine. Scientists are studying genetic markers like the CYP2E1 enzyme variant, which can identify people at 4.7 times higher risk of liver damage from alcohol and acetaminophen. In the near future, a simple blood test could tell you if you’re genetically more vulnerable to these interactions. But until then, the safest choice is clear: when in doubt, leave the alcohol out.Can I have one drink while taking painkillers?
It depends on the medication. For acetaminophen (Tylenol), even one drink can increase liver damage risk. For NSAIDs like ibuprofen, one drink raises your chance of stomach bleeding. For opioids or benzodiazepines, any amount can be deadly. If you’re unsure, don’t risk it.
Does alcohol make antidepressants less effective?
Yes. Alcohol can worsen depression symptoms and reduce how well SSRIs like Prozac or Zoloft work. It also increases drowsiness, dizziness, and the risk of falls. Even if you feel fine, alcohol is working against your treatment.
Is it safe to drink after finishing antibiotics?
For most antibiotics, yes-after a day or two. But for metronidazole (Flagyl), tinidazole, or certain others, you must wait at least 72 hours after your last dose. Drinking sooner can cause severe nausea, vomiting, fast heartbeat, and chest pain.
Why are older adults more at risk?
As we age, our liver and kidneys process alcohol and medications slower. We also tend to take more medications-on average, 14 prescriptions a year after 65. This increases the chance of dangerous interactions. The Beers Criteria lists 30 medications that are especially risky for seniors when mixed with alcohol.
Can I drink alcohol while taking blood pressure medicine?
It can be dangerous. Alcohol can cause your blood pressure to drop suddenly, especially when standing up. This increases your risk of dizziness, falls, and injuries. For older adults or those on multiple blood pressure drugs, even one drink can be risky. Always check with your doctor.
What should I do if I accidentally mixed alcohol and medication?
If you feel dizzy, confused, have trouble breathing, chest pain, or severe nausea, call emergency services immediately. Even if you feel fine, call your pharmacist or doctor. Some reactions take hours to show up. Better safe than sorry.
Are herbal supplements safe with alcohol?
No. Many herbal products like kava, valerian, or St. John’s wort can interact with alcohol. Kava and valerian can increase drowsiness and liver damage risk. St. John’s wort can raise serotonin levels, and alcohol can worsen side effects. Treat herbal supplements like real medicine-they can be just as dangerous.
Jimmy Kärnfeldt
December 10, 2025 AT 22:40Man, I never realized how many meds I’m on that could turn a Friday night glass of wine into an ER trip. I take Tylenol for my back and a beer after work-now I’m second-guessing every sip. Guess I’ll start switching to sparkling water. My liver’s probably been screaming for years and I just couldn’t hear it over the Netflix.
Michaux Hyatt
December 11, 2025 AT 15:58Big shoutout to pharmacists-they’re the real MVPs here. I asked mine about mixing my blood pressure med with wine, and she pulled up a chart showing exactly how much it could drop my BP. She even printed me a little cheat sheet. Doctors don’t have time. Pharmacists do. Talk to them before you pour.
Raj Rsvpraj
December 12, 2025 AT 11:49Stop being so fragile!
ALCOHOL IS SACRED!
YOU ARE NOT SACRED!
Jack Appleby
December 14, 2025 AT 07:55Let’s be precise: the CYP2E1 polymorphism doesn’t just increase risk-it confers a 4.7-fold relative risk increase (95% CI: 3.9–5.6) for hepatotoxicity when acetaminophen is co-ingested with ethanol. And yet, the FDA’s labeling remains woefully inadequate. You’re not just ‘at risk’-you’re a walking pharmacokinetic disaster if you’re homozygous for rs4646437. And no, ‘one drink’ isn’t a threshold-it’s a probabilistic trigger. Your liver doesn’t care about your intentions.
Frank Nouwens
December 15, 2025 AT 20:24It is, without question, a matter of considerable public health concern that the intersection of alcohol consumption and pharmaceutical use remains under-discussed in primary care settings. The data, as presented, is both compelling and alarming. One might reasonably posit that a standardized, system-wide pharmacovigilance protocol-perhaps integrated into EHR alerts-would yield a measurable reduction in adverse events. I propose, for consideration, a national campaign: ‘When in Doubt, Skip the Drink.’
Kaitlynn nail
December 17, 2025 AT 07:01…I need a nap.
Aileen Ferris
December 17, 2025 AT 13:07Michelle Edwards
December 17, 2025 AT 20:18I used to think ‘just one’ was harmless. Then my mom had a fall after a glass of wine and her blood pressure med. Broke her hip. She’s 72. We didn’t know the combo was risky.
Now I check every single thing with her pharmacist before she even opens a bottle.
It’s not about being paranoid. It’s about loving someone enough to ask the question-even when they roll their eyes.
Neelam Kumari
December 18, 2025 AT 17:07Queenie Chan
December 19, 2025 AT 02:22Okay, but what about kombucha? It’s got like 0.5% alcohol. Is that a problem? What about vanilla extract? Or cough syrup? And what if I’m on a low-dose SSRI and I have a single sip of sangria at a wedding? Am I basically signing a death warrant?
Also, does this apply to CBD tinctures? Because I’ve been using those with my evening tea and now I’m panicking.
Someone please tell me if my chamomile + lavender + alcohol + melatonin + gabapentin combo is a bomb waiting to go off. I need to know before I go to bed tonight.
Ariel Nichole
December 20, 2025 AT 08:29Thanks for writing this. I’m the author of the post. I’ve been sober for 11 months since my dad died from mixing his pain meds with whiskey. He never knew it could kill him. I’m not here to shame anyone-I just want people to know: you don’t have to lose someone to learn this.
Ask the pharmacist. Wait 72 hours. Skip the drink.
It’s not about giving up joy. It’s about keeping it alive.