When you're in the middle of a urinary tract infection (UTI), every trip to the bathroom feels like a battle. Burning, urgency, sharp pain-none of it waits for a convenient time. You might have been prescribed an antibiotic to kill the bacteria, but you're still hurting. That’s where phenazopyridine comes in. It doesn’t cure the infection. But it makes the pain bearable while your body fights it off.
What phenazopyridine actually does
Phenazopyridine is a urinary analgesic. That means it targets pain in the urinary tract, not the infection itself. It works by numbing the lining of the bladder and urethra. Think of it like a local anesthetic for your urinary system. You’ll feel relief from burning, urgency, and discomfort-often within 20 to 30 minutes after taking it.
But here’s the catch: it doesn’t kill bacteria. It doesn’t reduce fever. It doesn’t shorten the infection. If you take phenazopyridine alone, the infection will keep spreading. That’s why it’s never prescribed by itself. It’s always paired with an antibiotic like nitrofurantoin, trimethoprim-sulfamethoxazole, or ciprofloxacin.
Doctors use this combo because it addresses two problems at once: the cause (bacteria) and the symptoms (pain). Without phenazopyridine, many patients would stop their antibiotics early because the pain is too intense. With it, they’re more likely to finish the full course-which is critical to prevent resistant infections.
How antibiotics fight the infection
Antibiotics are the real cure. They attack the bacteria causing the UTI-usually E. coli, which makes up 80% of cases. Different antibiotics work in different ways. Nitrofurantoin stays concentrated in the urine and kills bacteria as they pass through. Trimethoprim-sulfamethoxazole blocks bacterial growth by interfering with folate production. Ciprofloxacin disrupts DNA replication in the bacteria.
The choice depends on your health history, local resistance patterns, and whether you’ve had UTIs before. In Australia, nitrofurantoin is often first-line for uncomplicated UTIs because resistance is still low. In recurrent cases, doctors might switch to fosfomycin or pivmecillinam.
Antibiotics usually start working within 24 to 48 hours. But you still need to take the full prescription-even if you feel better. Stopping early lets surviving bacteria multiply and become stronger. That’s how drug-resistant UTIs form.
Why the combination matters
Imagine trying to run a marathon with a broken ankle. You can keep going, but it’s painful, slow, and you’re more likely to give up. Phenazopyridine is like a brace. It doesn’t fix the ankle, but it lets you keep moving.
Studies show that patients who take phenazopyridine with antibiotics report significantly better comfort scores. One 2023 trial in the Journal of Antimicrobial Chemotherapy found that 78% of patients on the combo reported "significant pain relief" within 24 hours, compared to just 32% on antibiotics alone.
This isn’t just about comfort. It’s about compliance. People who feel better faster are more likely to finish their antibiotics. That reduces the risk of kidney infections, sepsis, and antibiotic resistance.
Phenazopyridine is also used in hospitals for post-surgical UTIs and after catheter insertion. It’s not just for home use-it’s part of standard care in many clinical settings.

What to expect when you take them together
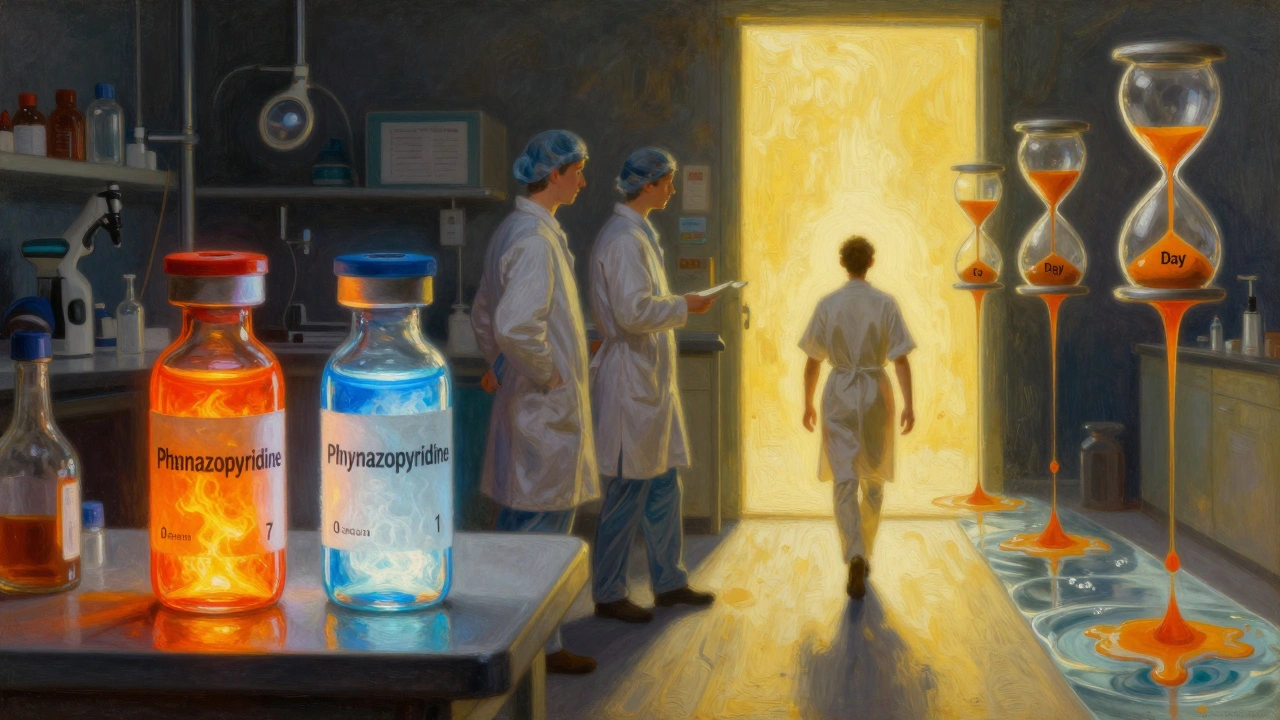
When you start this combo, here’s what usually happens:
- Day 1: You take your first dose of phenazopyridine. Pain eases within an hour. Your urine turns bright orange or red. Don’t panic-that’s normal. It’s harmless, but it can stain clothing and contact lenses.
- Day 2-3: Antibiotics begin killing bacteria. You still feel some discomfort, but less. Urgency drops. You might notice less frequent trips to the bathroom.
- Day 4-7: Pain fades. Urine color returns to normal. You feel like yourself again.
Most people feel significantly better by day 3. But don’t stop phenazopyridine early just because the pain is gone. It’s typically taken for only 2 days, even if you’re still on antibiotics. Longer use increases the risk of side effects.
Side effects and safety
Phenazopyridine is generally safe for short-term use. But it’s not for everyone.
Common side effects include:
- Orange-red urine (harmless)
- Headache
- Dizziness
- Stomach upset
Less common but serious side effects include:
- Yellowing of the skin or eyes (sign of liver stress)
- Shortness of breath
- Unusual tiredness or pale skin (sign of anemia)
If you have kidney disease, liver problems, or G6PD deficiency, phenazopyridine can be dangerous. It’s not recommended for children under 12 or pregnant women without close medical supervision.
Antibiotics have their own risks. Diarrhea, yeast infections, and allergic reactions are possible. Never share antibiotics or use leftovers from a previous infection. Each UTI is unique, and using old prescriptions can lead to treatment failure.
What not to do
There are three big mistakes people make with this combo:
- Stopping phenazopyridine too soon. If you feel better on day 2, you might think you don’t need it anymore. But the pain can return if the inflammation hasn’t fully settled. Stick to the 2-day window your doctor gave you.
- Using it as a substitute for antibiotics. Some people buy phenazopyridine over the counter (in some countries) and think it’s enough. It’s not. You’re just masking symptoms while the infection spreads.
- Ignoring warning signs. If you still have fever, back pain, nausea, or vomiting after 48 hours on antibiotics, call your doctor. That could mean the infection has reached your kidneys.
Also, don’t drink alcohol while taking phenazopyridine. It can worsen dizziness and liver stress. And avoid taking it with other painkillers like ibuprofen unless your doctor says it’s okay-they can increase kidney strain.
When to see a doctor
You don’t need to wait for symptoms to get worse before seeking help. Go to a doctor if:
- You’re pregnant
- You’re over 65
- You have diabetes or a weakened immune system
- You’ve had three or more UTIs in the last year
- Your symptoms don’t improve after 48 hours of antibiotics
These aren’t just "risk factors"-they’re red flags. UTIs in older adults or people with chronic conditions can turn into sepsis quickly. A simple urine test can confirm the infection and guide the right antibiotic.
Alternatives and what’s next
Not everyone can take phenazopyridine. If you have kidney issues or are allergic, your doctor might suggest:
- Increased hydration-drinking 2-3 liters of water a day helps flush bacteria
- Warm compresses on the lower abdomen to ease cramping
- Pain relievers like paracetamol (acetaminophen) for general discomfort
- Probiotics to support healthy bladder flora after antibiotics
Some people ask about cranberry supplements. Evidence is mixed. While cranberry may help prevent UTIs in some, it doesn’t treat active infections. Don’t rely on it as a substitute for antibiotics.
For recurrent UTIs, doctors may recommend low-dose antibiotics for prevention, or vaginal estrogen for postmenopausal women. In rare cases, imaging tests like ultrasounds are needed to check for structural problems.
Final thoughts
Phenazopyridine and antibiotics aren’t just a pair-they’re a team. One handles the pain. The other handles the infection. Together, they get you back to normal faster and safer.
Don’t see phenazopyridine as a shortcut. See it as a tool that makes the real treatment possible. Finish your antibiotics. Stay hydrated. Watch for warning signs. And if your pain comes back after you’ve finished both, don’t ignore it. That’s your body telling you something’s still wrong.
Can phenazopyridine cure a UTI on its own?
No, phenazopyridine cannot cure a UTI. It only relieves pain and discomfort by numbing the urinary tract. It does not kill bacteria. A bacterial UTI requires an antibiotic to clear the infection. Taking phenazopyridine alone can delay proper treatment and lead to complications like kidney infection.
How long should I take phenazopyridine?
Phenazopyridine is typically taken for only 2 days, even if you’re still on antibiotics. It’s meant for short-term symptom relief while your body responds to the antibiotic. Taking it longer than recommended increases the risk of side effects like liver damage or blood disorders. Always follow your doctor’s instructions.
Why does my urine turn orange when I take phenazopyridine?
The orange or red color is a normal side effect of phenazopyridine. It’s caused by the dye-like compounds in the drug being filtered out by your kidneys. It’s harmless and will go away once you stop taking it. However, it can stain clothing and contact lenses, so be careful. If your urine turns dark brown or you notice other symptoms like jaundice, contact your doctor immediately.
Can I take phenazopyridine with ibuprofen or paracetamol?
Paracetamol (acetaminophen) is generally safe to take with phenazopyridine for general pain or fever. Ibuprofen and other NSAIDs can be used cautiously, but they may increase the risk of kidney strain, especially if you’re dehydrated or have existing kidney issues. Always check with your doctor before combining medications.
Is phenazopyridine safe during pregnancy?
Phenazopyridine is not recommended during pregnancy unless specifically prescribed by a doctor. While some studies suggest low risk in the second trimester, it can cross the placenta and may affect the baby’s blood cells. Pregnant women with UTIs are usually treated with antibiotics like nitrofurantoin or cephalexin, and pain relief is managed with paracetamol instead.
What should I do if my UTI symptoms return after finishing antibiotics?
If symptoms come back after finishing your antibiotics, don’t assume it’s the same infection. You may have a different strain of bacteria, a resistant infection, or an underlying issue like a kidney stone or bladder abnormality. See your doctor for a new urine test and possibly a culture to identify the exact bacteria. Self-treating with leftover antibiotics can make the problem worse.

Karandeep Singh
December 2, 2025 AT 17:19phenazopyridine is just a dye that makes your pee look like a highlighter and pretends to help
Erin Nemo
December 4, 2025 AT 02:42orange pee is wild but at least i knew i took my med lol
Edward Hyde
December 5, 2025 AT 08:01so let me get this straight-you’re telling me we pay big pharma to sell us a chemical that turns your piss neon and calls it medicine? brilliant. absolute corporate genius. next they’ll sell us glitter to fix our kidneys.
Rachel Stanton
December 7, 2025 AT 06:57Really appreciate how this breaks down the synergy between symptom relief and pathogen eradication. Phenazopyridine isn’t a band-aid-it’s a bridge. The real win is adherence: when pain is manageable, patients complete antibiotics, which directly reduces resistance rates. This is clinical pragmatism at its finest. Also, the 2-day limit is critical-longer use risks methemoglobinemia, especially in G6PD-deficient individuals. Always check labs if used beyond 48h in high-risk populations.
Debbie Naquin
December 8, 2025 AT 17:06The phenomenology of urinary pain is undertheorized in medical discourse. Phenazopyridine doesn’t cure-it epoche’s sensation. It brackets the bodily suffering, allowing the patient to re-engage with the world while the antibiotic performs its ontological negation of the bacterial other. The orange urine? A semiotic marker of pharmacological intervention-a visible signifier of the body’s internal war. We mistake symptom suppression for healing, but here, suppression enables healing. It’s not palliative-it’s epistemic.
Lauryn Smith
December 9, 2025 AT 21:22if you’re pregnant or have kidney issues, skip phenazopyridine. paracetamol and water are your friends. and yes, cranberry juice won’t fix an active infection but it won’t hurt either if you like the taste.
Suzanne Mollaneda Padin
December 11, 2025 AT 02:27As someone from the US who’s had three UTIs in two years, this is spot-on. I used to stop antibiotics because the pain was unbearable. Phenazopyridine made the difference between finishing my script and ending up in the ER. Also, the orange pee freaked me out the first time-I thought I was bleeding. Glad I didn’t panic. Just keep drinking water.
Amber-Lynn Quinata
December 11, 2025 AT 10:55Why do people still take antibiotics like they’re candy? 😒 You think one course makes you immune? No. It makes you a walking superbug factory. And phenazopyridine? It’s just a distraction. If you’re in that much pain, maybe you shouldn’t have waited 3 days to see a doctor. 🤦♀️
Charlotte Collins
December 11, 2025 AT 14:05Let’s not romanticize this. Phenazopyridine is a Band-Aid on a gunshot wound. It’s a corporate profit engine disguised as compassion. The real problem? The medical system incentivizes quick fixes over root-cause resolution. UTIs recur because we don’t investigate biofilm formation, catheter hygiene, or pelvic floor dysfunction. We hand out antibiotics and dye, then wonder why resistance is rising. It’s not a treatment-it’s a systemic failure with a bright orange label.
ariel nicholas
December 12, 2025 AT 02:04So, in America, we’ve reduced medicine to a two-step dance: take the dye, take the poison, and pray. Meanwhile, in Germany, they use herbal remedies and physical therapy. In Japan, they’ve got acupuncture protocols for cystitis. But no-here, we need a $40 pill that turns your urine into a traffic cone. This isn’t healthcare-it’s performance art for shareholders.