What Exactly Is Otitis Media?
Otitis media is an infection or inflammation of the middle ear, the space behind the eardrum that’s normally filled with air. It’s one of the most common reasons parents take their kids to the doctor - especially between 3 months and 3 years old. In fact, more than 80% of children will have at least one middle ear infection before their third birthday. While adults can get it too, kids are far more likely because their Eustachian tubes - the tiny channels that connect the middle ear to the back of the throat - are shorter, more horizontal, and not as good at draining fluid.
When a cold, flu, or allergy causes swelling in the throat, those tubes get blocked. Fluid builds up behind the eardrum, and that’s when bacteria or viruses - like Streptococcus pneumoniae, Haemophilus influenzae, or respiratory viruses - move in and cause infection. This leads to pressure, pain, fever, and sometimes even temporary hearing loss.
How Do You Know It’s an Ear Infection?
Not every ear tug or fuss means an ear infection. Many parents panic when their toddler pulls at their ear, but that alone isn’t enough. The real signs are more specific:
- Sharp, persistent ear pain - often worse at night
- Fever above 38.5°C (101.3°F)
- Crying more than usual, especially when lying down
- Difficulty sleeping or eating
- Fluid draining from the ear (this can mean the eardrum has burst - still not an emergency, but needs checking)
- Loss of balance or seeming unresponsive to quiet sounds
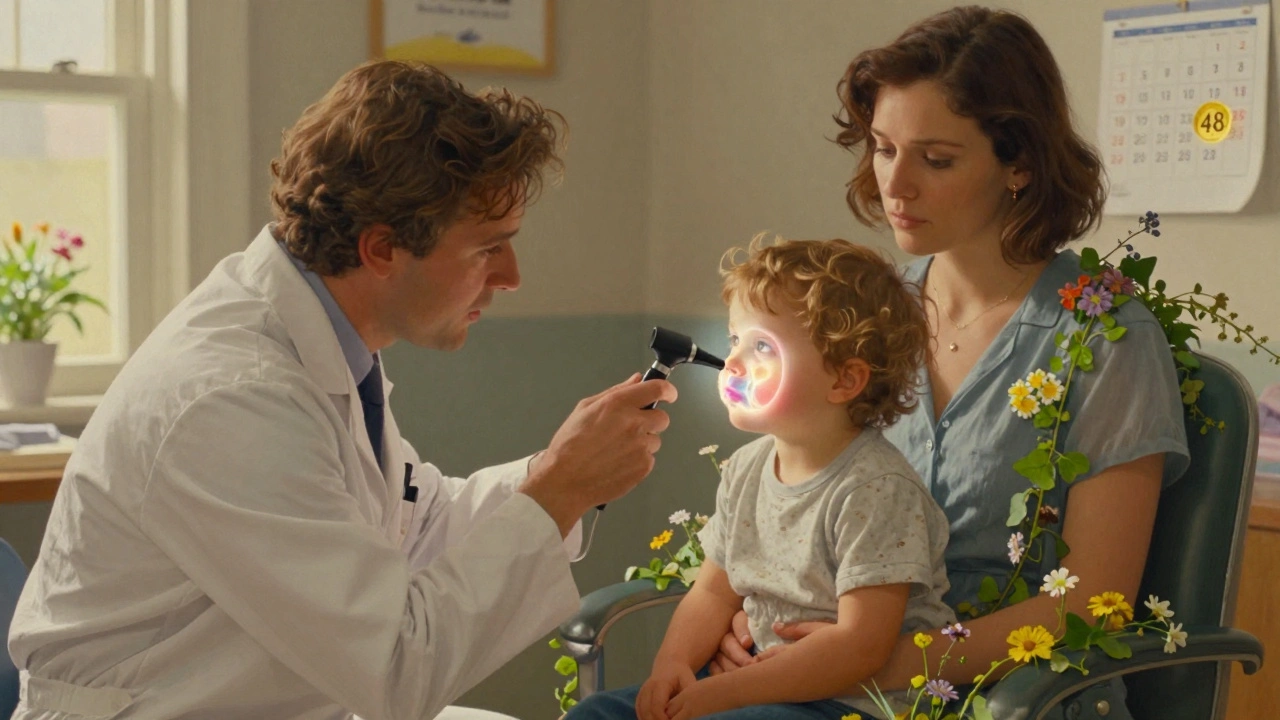
Doctors diagnose it using a tool called a pneumatic otoscope. It lets them see if the eardrum is red, bulging, and doesn’t move when air is gently puffed into the ear. That’s the classic sign of acute otitis media (AOM). If fluid is stuck behind the eardrum but there’s no infection, that’s called otitis media with effusion (OME). OME doesn’t need antibiotics - it often clears on its own within weeks or months.
Antibiotics: When They Work - and When They Don’t
Here’s the hard truth: most ear infections get better without antibiotics. Studies show that about 80% of kids with mild to moderate AOM recover fully within 3 days without any antibiotics. The body’s immune system can handle it.
But antibiotics aren’t useless. They’re crucial in specific cases:
- Children under 6 months with confirmed infection
- Kids 6 to 23 months with severe symptoms - fever over 39°C or pain lasting more than 48 hours
- Children 2 years and older with severe pain or high fever
- Any child with a ruptured eardrum and pus drainage
- Children with weakened immune systems or other health conditions
For everyone else, especially older kids with mild symptoms, doctors now recommend watchful waiting. That means managing pain, watching closely for 48 to 72 hours, and only starting antibiotics if things get worse.
What Antibiotics Are Used - and Why Amoxicillin Is First Choice
When antibiotics are needed, amoxicillin is the go-to. It’s cheap, safe, and effective against the most common bacteria causing ear infections. The standard dose is 80-90 mg per kilogram of body weight per day, split into two doses. For kids under 2, it’s usually given for 10 days. For older kids with mild cases, 5 to 7 days may be enough.
If a child is allergic to penicillin, alternatives include:
- Cefdinir - an oral cephalosporin
- Ceftriaxone - a single shot, used if the child can’t take oral meds
- Azithromycin - a 5-day course, though less effective against some strains
Amoxicillin-clavulanate (Augmentin) is often used if the infection doesn’t improve or if the child has had multiple infections. But it’s not first-line because it increases the risk of diarrhea and contributes to antibiotic resistance.
Antibiotic resistance is real. In the U.S., 30-50% of Streptococcus pneumoniae strains are resistant to penicillin. That’s why high-dose amoxicillin is preferred - it overcomes many of these resistant bugs.
Pain Management: The Most Important First Step
Whether or not you use antibiotics, controlling pain is the top priority. A child in pain can’t sleep, eat, or calm down. The best tools are simple:
- Ibuprofen - 5-10 mg per kg every 6-8 hours
- Acetaminophen - 10-15 mg per kg every 4-6 hours
Many parents report that ibuprofen works better than acetaminophen for ear pain because it reduces inflammation too. Don’t wait for the fever to spike - start pain relief early. Warm compresses on the ear can help, and some doctors recommend over-the-counter ear drops like Auralgan, but only if the eardrum isn’t ruptured.
One parent on Reddit shared: “Ibuprofen every 6 hours turned my crying 18-month-old into a sleepy, calm kid within an hour. We waited 48 hours and the infection cleared on its own.”
What to Watch For - Red Flags That Need Immediate Care
Most ear infections are harmless and resolve without trouble. But some signs mean you need to see a doctor right away:
- Fever above 40°C (104°F)
- Severe pain that doesn’t improve with painkillers
- Swelling behind the ear or drooping of the face
- Stiff neck, dizziness, or confusion
- Pus or bloody fluid draining from the ear
- Signs of hearing loss lasting more than a few weeks after the infection clears
If the eardrum bursts, don’t panic. It usually heals on its own within a week or two. Just keep the ear dry and avoid putting anything inside it.
Prevention: Vaccines, Breastfeeding, and Smoke-Free Homes
You can’t always prevent ear infections, but you can lower the risk:
- Pneumococcal vaccines - PCV13 and the newer 15-valent vaccine (Vaxneuvance) have cut vaccine-type ear infections by 34% or more
- Breastfeeding - Babies fed upright while breastfeeding have lower rates than bottle-fed babies lying flat
- No smoke exposure - Kids in homes with smokers have a 50% higher risk
- Limit daycare exposure - Kids in group care get infections more often, but this isn’t avoidable for many families
- Handwashing and flu shots - Reducing colds reduces ear infections
Probiotics? A 2022 Cochrane review looked at 13 studies and found no real benefit. Don’t waste money on them.

When Ear Infections Keep Coming Back
One in five kids gets recurrent ear infections - three or more in six months. This can be frustrating for families and lead to repeated antibiotic courses.
For these kids, doctors may consider:
- Ear tubes (tympanostomy tubes) - tiny cylinders placed in the eardrum to help drain fluid
- Long-term low-dose antibiotics - rarely used now, only in very specific cases
- Removing adenoids - if they’re swollen and blocking the Eustachian tubes
Most kids outgrow frequent ear infections by age 5 or 6, as their Eustachian tubes grow longer and more angled. But if hearing loss or speech delays are happening, early intervention is critical.
The Bigger Picture: Antibiotic Overuse and the Cost of Care
In the U.S., ear infections lead to over 15 million antibiotic prescriptions every year - second only to sore throats. That’s a huge driver of antibiotic resistance. In 2010, 68% of ear infection cases got antibiotics. By 2016, that dropped to 59%. Progress, but still too high.
Healthcare costs? Over $2.8 billion a year in the U.S. alone. That includes doctor visits, prescriptions, ER trips, and missed work for parents.
New tools are helping. Smart otoscopes like CellScope let parents take pictures of the eardrum and send them to the doctor. Office-based tympanometry (a test that measures eardrum movement) has cut unnecessary antibiotic use by 22% in young kids.
Experts predict that within five years, point-of-care tests will quickly identify whether an infection is bacterial or viral - and only give antibiotics when truly needed.
What Parents Should Remember
Ear infections are scary, especially when your child is crying and can’t sleep. But you’re not powerless.
- Don’t rush to antibiotics - pain control and watchful waiting often work just as well
- Use ibuprofen or acetaminophen - not just for fever, but for pain
- Know the red flags - when to call the doctor
- Protect your child with vaccines and smoke-free air
- Fluid behind the ear (OME) isn’t an infection - it doesn’t need antibiotics
- Recurrent infections? Talk to your doctor about long-term options
The goal isn’t to avoid antibiotics at all costs. It’s to use them wisely - when they’ll actually help, and not when they’ll just cause side effects or make superbugs stronger.

Fern Marder
December 3, 2025 AT 14:56Carolyn Woodard
December 4, 2025 AT 08:05John Webber
December 4, 2025 AT 14:32Elizabeth Farrell
December 5, 2025 AT 06:45Saravanan Sathyanandha
December 6, 2025 AT 08:17alaa ismail
December 7, 2025 AT 08:26ruiqing Jane
December 8, 2025 AT 00:50Shubham Pandey
December 8, 2025 AT 02:17Sheryl Lynn
December 9, 2025 AT 09:30Paul Santos
December 9, 2025 AT 23:47Eddy Kimani
December 11, 2025 AT 16:44Chelsea Moore
December 12, 2025 AT 16:01John Biesecker
December 13, 2025 AT 21:13Genesis Rubi
December 14, 2025 AT 07:38Doug Hawk
December 14, 2025 AT 13:35