Glomerulonephritis is a condition where your immune system mistakenly attacks the tiny filters in your kidneys. First documented in 1877 by German pathologist Friedrich Daniel von Recklinghausen, this immune-mediated disorder affects about 12.5 per 100,000 people annually in the United States. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) reports that glomerulonephritis accounts for 10-15% of all end-stage kidney disease cases in the US, leading to thousands of new dialysis patients each year.
How the kidney filters work
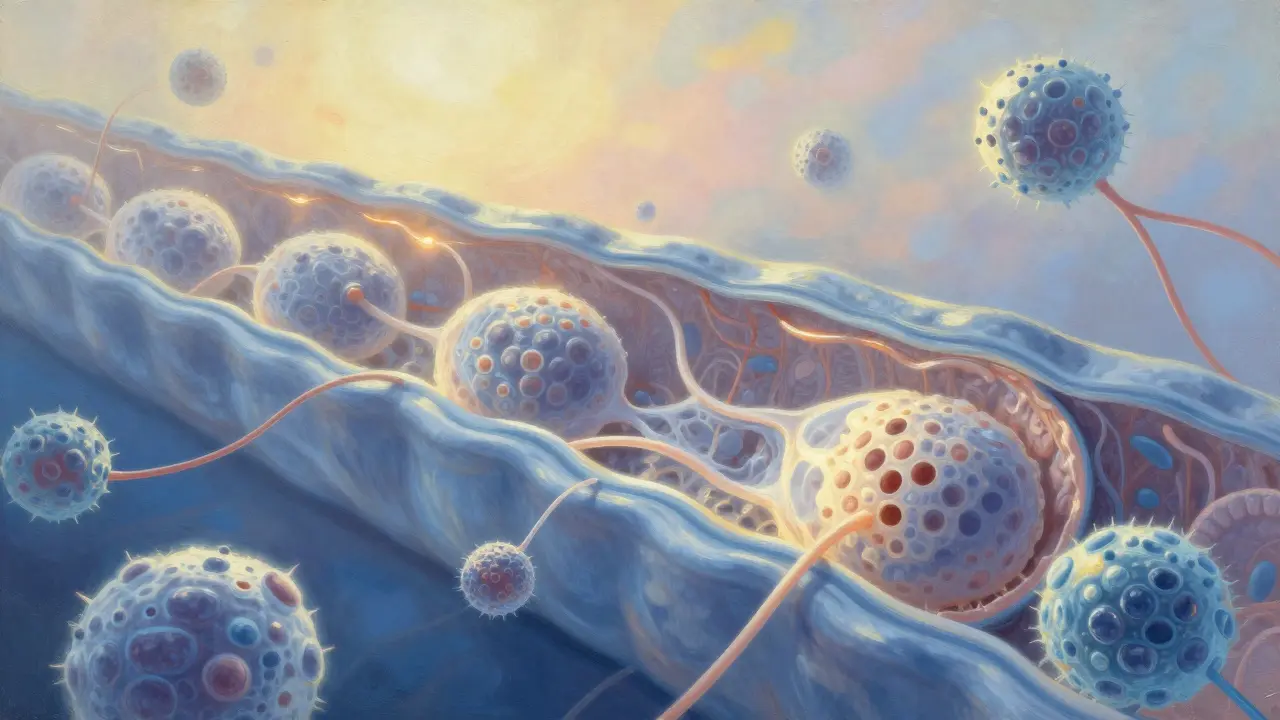
The glomeruli are the kidney's microscopic filters, each made up of three critical layers. From the inside out, there's the endothelial glycocalyx and cells lining the blood vessels, then the glomerular basement membrane (GBM), and finally podocytes - specialized cells that wrap around the capillaries. As explained in Nature Reviews Immunology (2022), "the filtration barrier encompasses, from the inside to the outside, the endothelial glycocalyx, glomerular endothelial cells, glomerular basement membrane and visceral epithelial cells (podocytes)." When this barrier gets damaged by immune attacks, proteins and blood leak into urine, and the kidneys can't filter waste properly. Imagine a sieve with holes - that's what happens when the immune system attacks these delicate structures.
Types of glomerulonephritis
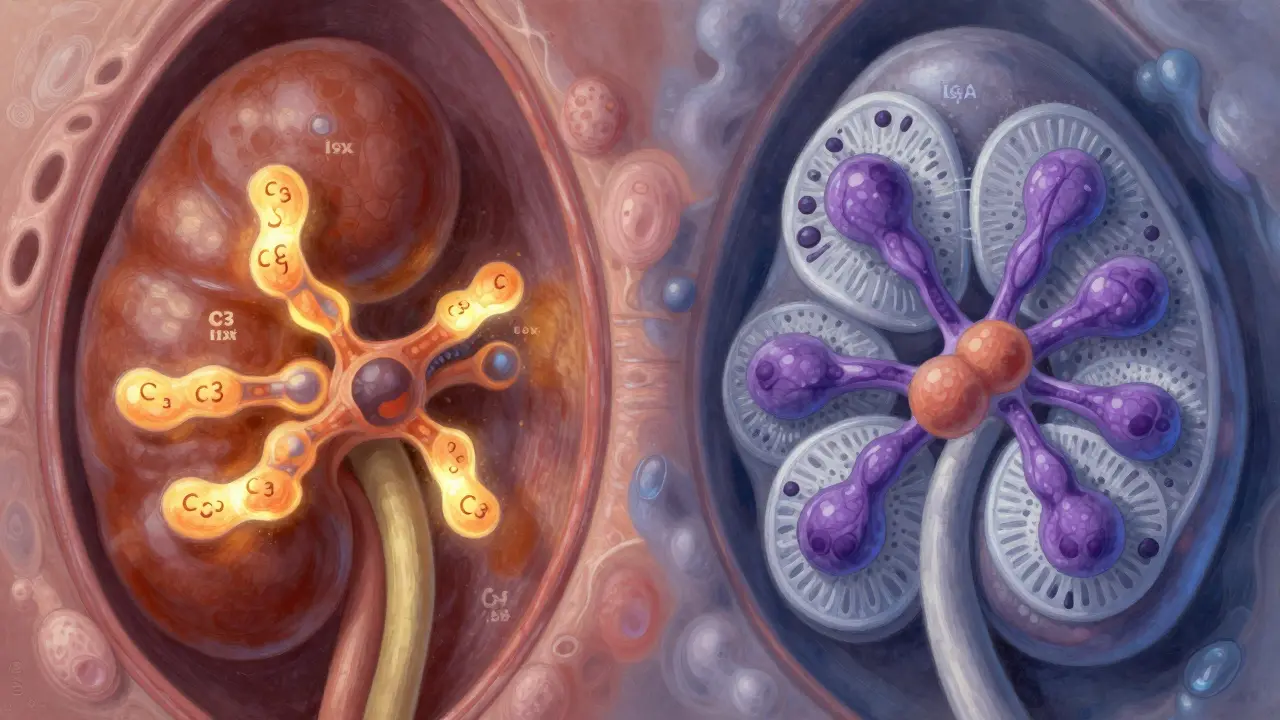
Glomerulonephritis isn't one-size-fits-all. Different types exist based on how the immune system attacks. For example, C3 Glomerulonephritis (C3G) happens when the complement system - part of the immune defense - goes haywire. In C3G, C3 protein builds up in the glomeruli at 3-5 times normal levels, causing inflammation. According to ERKNet (2023), about 60-70% of C3G cases involve autoantibodies against complement proteins. On the other hand, Immune Complex-Mediated Membranoproliferative GN (IC-MPGN) involves immune complexes (antibodies bound to antigens) getting stuck in the glomeruli. Biopsy studies show these deposits in 95% of IC-MPGN cases. Another common type is IgA nephropathy, the most prevalent primary GN worldwide. In North America, it affects roughly 2.5 per 100,000 people annually, with 20-40% progressing to kidney failure over 20 years. Lupus nephritis, which occurs in 50-60% of systemic lupus erythematosus patients, is another major form. With current treatments, 70-80% of lupus nephritis patients maintain kidney function for 10 years.
Symptoms of glomerulonephritis
Symptoms vary depending on whether it's nephritic or nephrotic syndrome. Nephritic syndrome includes blood in urine (making it pink or cola-colored), high blood pressure, reduced urine output, and swelling in legs or face. Nephrotic syndrome features foamy urine from protein loss, severe swelling (edema), high cholesterol, and low blood protein levels. Many patients also experience extreme fatigue - 65% report this as a major issue according to the American Kidney Fund. Online forums like Inspire.com show 78% of posts mention trouble managing edema, while 63% complain about medication side effects - particularly from corticosteroids. A Reddit thread in March 2023 shared stories of patients waiting an average of 4.2 months for a diagnosis, with 32% seeing three or more specialists before getting answers.
Diagnosing glomerulonephritis
Diagnosing GN usually requires a kidney biopsy - a procedure where a small tissue sample is taken from the kidney. While essential, this test carries risks: 3-5% complication rate including bleeding or pain, according to American Society of Nephrology guidelines. Interpreting biopsy results is complex. Nephropathologists need 5-7 years of specialized training to distinguish between different GN subtypes. The process isn't just about tissue analysis; it also involves blood tests for complement proteins and immune markers. For instance, C3G diagnosis often requires immunofluorescence staining to detect abnormal C3 deposits. The challenge is real. One patient shared on a support forum: "I had blood in my urine for months before anyone took it seriously. It took three doctors and two biopsies to get a clear answer."
Treatment options
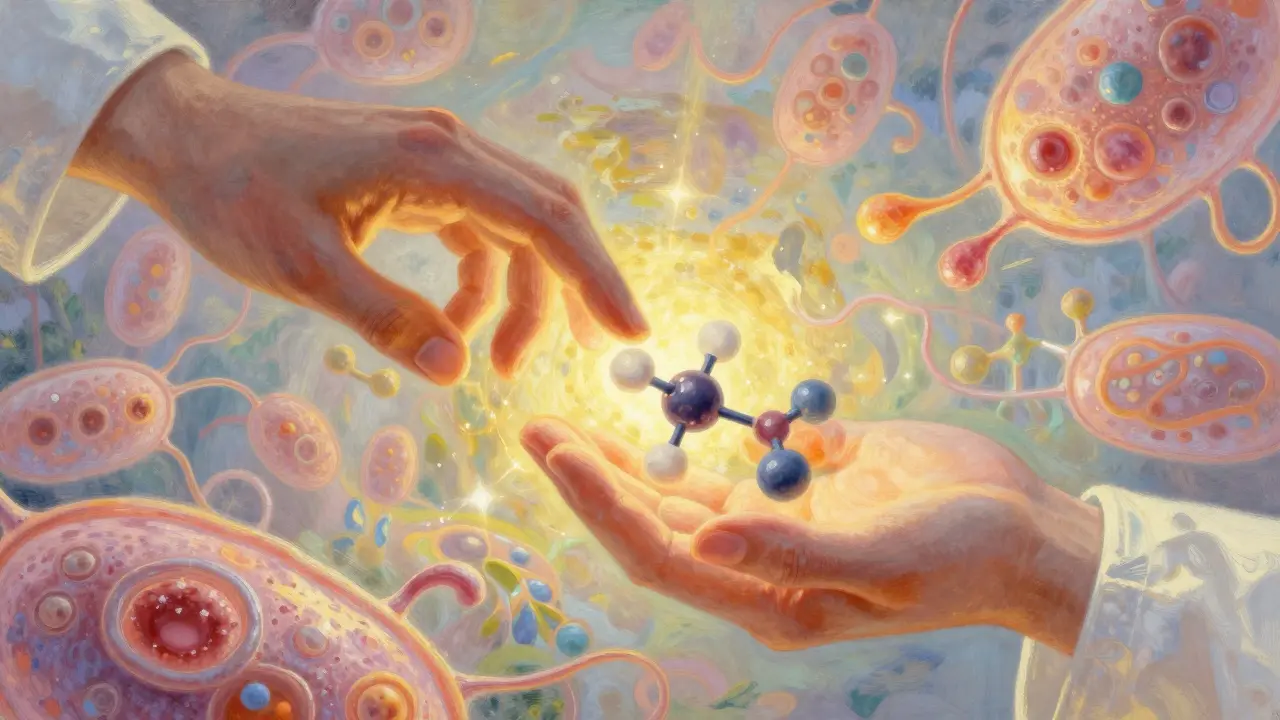
Current treatments often start with corticosteroids like prednisone. While 60-80% of patients respond initially, 30-50% experience serious side effects within a year. The NEPTUNE study published in Clinical Journal of the American Society of Nephrology (2023) reports weight gain in 72% of patients, increased infection risk in 35%, and bone density loss in 28%. Newer therapies are emerging. Eculizumab, used for C3G, reduces proteinuria but costs around $500,000 annually. In February 2023, the FDA granted breakthrough therapy designation to iptacopan (Novartis) for C3G after trials showed a 52% reduction in proteinuria. However, access remains unequal. KDIGO's 2023 guidelines note patients in low-income countries have 70% less access to advanced diagnostics and 90% less to novel treatments compared to high-income regions.
The future of glomerulonephritis treatment
Research is moving toward personalized treatments. Dr. Richard Lafayette from Stanford University predicts in the Journal of the American Society of Nephrology (2023) that "within 5 years, genetic and proteomic profiling will guide therapy selection for GN patients, potentially increasing treatment efficacy from 60-70% to over 85%." The European Renal Association's 2023 guidelines now use molecular biomarkers alongside traditional biopsy analysis, improving treatment response prediction accuracy to 85%. But challenges persist. The global GN treatment market is growing rapidly - projected to reach $4.7 billion by 2028 - yet equitable access remains a critical issue. As Dr. Laura Barisoni noted in the Journal of the American Society of Nephrology (2023), "novel therapies aimed at podocyte repair could offer benefits without the toxicities of current immunosuppressants," but scaling these solutions globally is still a hurdle.
What is the main cause of glomerulonephritis?
The main cause varies by type. In C3 Glomerulonephritis (C3G), it's often due to dysregulation of the complement system, with autoantibodies like C3 nephritic factor (C3NeF) present in 60-70% of cases. In IgA nephropathy, immune complexes containing IgA antibodies build up in the glomeruli. For lupus nephritis, it's part of systemic lupus erythematosus where autoantibodies attack the kidneys. Each type has a different immune mechanism, but all involve the immune system mistakenly targeting kidney filters.
How is glomerulonephritis diagnosed?
Diagnosis typically starts with urine and blood tests showing protein or blood in urine, high creatinine levels, or low albumin. However, a kidney biopsy is usually required for confirmation. During a biopsy, a small kidney tissue sample is taken and examined under a microscope. Pathologists look for specific patterns like immune deposits or complement proteins. Blood tests for complement levels and autoantibodies also help distinguish between types like C3G or IC-MPGN. The process can take several weeks and sometimes requires multiple specialists.
What are common symptoms of glomerulonephritis?
Symptoms depend on whether it's nephritic or nephrotic syndrome. Nephritic syndrome includes blood in urine (making it pink or cola-colored), high blood pressure, reduced urine output, and swelling in legs or face. Nephrotic syndrome features foamy urine from protein loss, severe swelling (edema), high cholesterol, and low blood protein levels. Many patients also experience extreme fatigue - 65% report this as a major issue according to the American Kidney Fund. Some may also have nausea or shortness of breath from kidney dysfunction.
Can glomerulonephritis be cured?
Some forms can be managed effectively, but a complete cure isn't always possible. Post-streptococcal GN often resolves on its own within weeks, with 95% of children recovering fully. IgA nephropathy has no cure but can be controlled with medications like ACE inhibitors or immunosuppressants. For severe cases like C3G or lupus nephritis, treatments aim to slow progression. Early intervention improves outcomes - one patient reported starting rituximab within two months of diagnosis prevented dialysis need. However, 20-40% of IgA nephropathy cases progress to end-stage kidney disease over 20 years without proper management.
What are the side effects of current treatments?
Corticosteroids like prednisone are common first-line treatments but cause significant side effects. The NEPTUNE study (2023) found 72% of patients gain weight, 35% face higher infection risk, and 28% experience bone density loss within the first year. Other immunosuppressants can lead to increased cancer risk or organ toxicity. Newer drugs like eculizumab are expensive ($500k/year) and may cause side effects like meningococcal infections. Patients often balance treatment benefits against these risks, which is why personalized approaches are becoming essential.
How do C3 Glomerulonephritis and IgA nephropathy differ?
C3G involves abnormal activation of the complement system, leading to C3 protein buildup in the glomeruli. It's often linked to autoantibodies against complement proteins (C3NeF in 60-70% of cases). IgA nephropathy results from IgA immune complexes depositing in the glomeruli. While C3G typically shows dominant C3 deposits on biopsy, IgA nephropathy has IgA deposits. C3G often progresses faster to kidney failure, with 50-60% 10-year survival rate without treatment, compared to IgA nephropathy's 60-80% survival with treatment.
What new treatments are on the horizon?
Recent breakthroughs include iptacopan (Novartis), which the FDA approved for C3G in 2023 after showing 52% proteinuria reduction. Drugs targeting specific complement components, like factor D inhibitors, are in trials. The European Renal Association's 2023 guidelines now use molecular biomarkers alongside biopsies for better treatment prediction. Research is also focusing on podocyte repair therapies - Dr. Laura Barisoni highlights these could offer benefits without current immunosuppressant side effects. However, cost and access remain major barriers globally.
Niel Amstrong Stein
February 7, 2026 AT 13:36Glomerulonephritis is a stark reminder that our immune system isn't always a friend. It's like having a security guard who's gone rogue. 🤯 The complexity of the kidney's filtration system is incredible-three layers working in harmony until the immune system messes it up. This makes me think about how delicate balance we have in our bodies. Maybe we should focus more on preventing immune dysregulation rather than just treating symptoms after the fact.
Paula Sa
February 8, 2026 AT 22:56Thanks for sharing this thoughtful perspective. I've been following research on immune dysregulation and it's amazing how much we're learning about the complement system. The fact that C3G involves autoantibodies in 60-70% of cases is really important for targeted treatments. Hope more people understand how complex this is.
Mary Carroll Allen
February 9, 2026 AT 05:14Okay but like seriously we don't have better treatments yet. Theyre just throwing steroids at people and hoping for the best. The side effects are insane-weight gain, bone loss, infections. And the cost for new drugs like eculizumab is $500k a year. Thats ridiculous. We need to fix this system. #MedicalInjustice
Joey Gianvincenzi
February 11, 2026 AT 02:58It is imperative to address the systemic inequities in access to advanced diagnostics and novel treatments. The data presented clearly indicates that patients in low-income countries face 70% less access to diagnostics and 90% less to treatments. This is unacceptable and requires immediate global action. The current market-driven approach is failing those most in need.
Amit Jain
February 12, 2026 AT 17:40The article overlooks the 30-40% of C3G cases without autoantibodies. IgA nephropathy is more common yet gets less attention. This seems like biased reporting. $500k drugs are corporate greed. We need real solutions, not expensive band-aids.
Sarah B
February 13, 2026 AT 10:33US leads in medical research we need to fund more domestic studies stop relying on foreign data
Eric Knobelspiesse
February 15, 2026 AT 03:15The immune system attacking kidneys might be a symptom of bigger issues like environment or diet. We're all just trying to survive in this world but sometimes the body just gives up. We need to look at the bigger picture instead of just treating symptoms. But hey, what do I know? 😅
Heather Burrows
February 15, 2026 AT 20:38We've known about glomerulonephritis for decades. Progress has been slow. People aren't taking it seriously enough. I guess we'll see what happens.
Ariel Edmisten
February 15, 2026 AT 20:47Kidney filters are delicate. Immune attacks damage them. Treatments have side effects. Research is ongoing. We need better options. Simple as that.
Tola Adedipe
February 16, 2026 AT 01:23Collaboration is key. We need more global partnerships to improve access to treatments. But we also need to push for cheaper drugs. The current system is broken. Let's work together to fix it.
Ritu Singh
February 16, 2026 AT 05:29The complexity of glomerulonephritis underscores the importance of personalized medicine. By integrating genetic and proteomic data, we can tailor treatments to individual patients, reducing side effects and improving outcomes. This approach aligns with the future of nephrology, as highlighted in recent studies. However, equitable access remains a critical challenge that must be addressed.
Mark Harris
February 17, 2026 AT 08:48Let's stay positive! Research is moving fast. New drugs like iptacopan are showing promise. We're making progress, even if it's slow. Keep pushing for better treatments and support each other. We got this! 💪