CNS Depressant Interaction Risk Calculator
This tool helps assess the potential risk of combining cannabis with CNS depressants based on your specific situation.
Risk Assessment
Combining cannabis with prescription sedatives like benzodiazepines, opioids, or barbiturates isn’t just risky-it can be life-threatening. If you’re using medical cannabis for pain, anxiety, or sleep, and also take a sleeping pill, painkiller, or anti-anxiety medication, you’re not just doubling the drowsiness. You’re multiplying the danger.
How Cannabis Acts Like a CNS Depressant
Cannabis isn’t just a plant you smoke for relaxation. Its main psychoactive compound, delta-9-tetrahydrocannabinol (THC), directly slows down brain activity by binding to CB1 receptors in the central nervous system. This is the same mechanism used by drugs like Xanax, Valium, and opioids-but through different pathways. The result? Slowed reaction time, impaired memory, poor coordination, and deep sedation.Even small doses of THC-5 to 10 mg-can cause noticeable effects in experienced users. When you smoke or vape cannabis, those effects hit within minutes and peak around 30 minutes. If you eat an edible, it takes 30 to 90 minutes to kick in, but the high lasts much longer-up to 8 hours. That extended window increases the chance of accidental overlap with other depressants.
Unlike alcohol or prescription drugs, cannabis doesn’t always feel like a depressant. At low doses, some people report increased energy or alertness. But that’s misleading. Even when you feel "stimulated," your brain is still processing information slower than normal. That’s why mixing cannabis with sedatives is so dangerous-you don’t realize how impaired you are until it’s too late.
The Real Danger: Additive, Not Just Combined
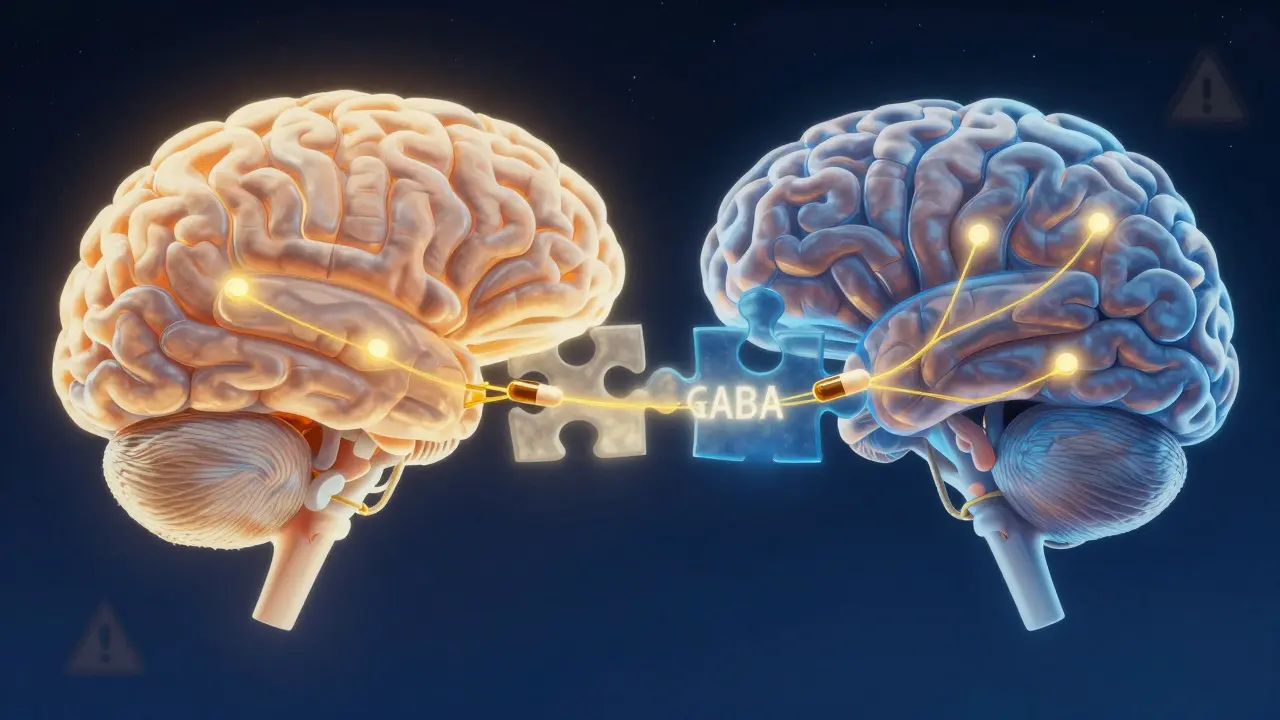
It’s not enough to say cannabis "adds" to the effects of other CNS depressants. The interaction is synergistic. That means the total effect is greater than the sum of each drug alone.Take benzodiazepines and THC. Both enhance GABA, the brain’s main calming neurotransmitter. When used together, they don’t just make you sleepy-they can shut down your breathing. A 2020 study in the Journal of Clinical Medicine found people using both had over three times the risk of ending up in the emergency room. Of those visits, 67% involved respiratory problems.
The risk is even worse with opioids. Both substances suppress the brainstem’s drive to breathe. Cannabis doesn’t just make opioids more sedating-it makes them more likely to stop your breathing entirely. There’s no safe threshold when these two are mixed. Even low-dose opioids combined with moderate THC can lead to fatal respiratory depression.
One Reddit user, u/AnxietyWarrior, described waking up on the bathroom floor after taking 0.5 mg of Xanax and one hit of 20% THC flower. Their oxygen levels had dropped to 82%. That’s dangerously low. Normal is above 95%. They didn’t pass out from being too high-they nearly died from stopped breathing.
Who’s at Highest Risk?
It’s not just recreational users. The biggest problem is medical patients managing chronic conditions. Older adults, especially those on multiple prescriptions, are at the greatest risk.A 2021 survey of 1,247 medical cannabis patients found that nearly 39% were also taking CNS depressants. Over 22% of them had experienced an episode of extreme sedation-so bad they needed medical help. Many didn’t realize the danger because their doctors never warned them.
Seniors are especially vulnerable. Their bodies process drugs slower. Their lungs and heart aren’t as resilient. A 65-year-old on opioids for back pain and a low-dose benzodiazepine for sleep could be walking a tightrope. Add even a small edible of 10% THC, and the risk of falling, confusion, or respiratory failure spikes.
Even people who think they’re "safe" because they use CBD aren’t out of the woods. While CBD-dominant products (with less than 0.3% THC) show fewer interactions in early studies, most medical cannabis products still contain noticeable THC. And if you’re using full-spectrum oil-common in pain and anxiety treatment-you’re still getting enough THC to cause problems.
What Doctors Are Saying
Medical experts are sounding the alarm. The American Society of Anesthesiologists says anyone using cannabis within 72 hours of surgery needs special monitoring. Why? Because anesthesia is a powerful CNS depressant. A 2021 study found cannabis users needed 20-25% more propofol to be put to sleep-but then had 37% more breathing problems waking up.The American Academy of Neurology warns that combining cannabis with benzodiazepines creates unpredictable effects on brain chemistry. What might work for one person-a little calm, better sleep-could send another into a blackout or respiratory arrest.
Dr. Igor Grant, who leads the Center for Medicinal Cannabis Research at UC San Diego, calls this one of the most under-recognized dangers in modern medicine. "We’re seeing older patients on pain meds, sleep aids, and now cannabis. No one connects the dots until someone ends up in the ICU."
Real Numbers, Real Consequences
The data doesn’t lie. In 2022, U.S. emergency departments recorded 7,842 visits involving cannabis and benzodiazepines. That’s a 42% jump from just three years earlier. Most of these cases involved accidental overdoses-people thought they were being careful, but didn’t realize how the drugs amplified each other.Meanwhile, the FDA and European Medicines Agency now require warning labels on all prescription CNS depressants that mention cannabis. It’s no longer an afterthought-it’s a required safety note.
And it’s not just the U.S. States with medical cannabis programs are taking action. California now requires all doctors who certify patients for medical marijuana to complete a two-hour training on drug interactions. Since 2022, high-risk combinations have dropped by 28%.

What to Do If You’re Using Both
If you’re taking a CNS depressant and using cannabis-whether for medical or recreational reasons-here’s what you need to do:- Stop assuming it’s safe. Just because you’ve done it before doesn’t mean it won’t kill you next time.
- Talk to your doctor. Don’t hide your cannabis use. If you’re on opioids, benzodiazepines, sleeping pills, or muscle relaxants, your doctor needs to know.
- Avoid high-THC products. Anything over 15% THC significantly increases risk. Stick to low-dose options if you must use both.
- Never mix with alcohol. Alcohol plus cannabis plus a prescription depressant is a triple threat. This combination has killed people.
- Stagger your doses. If you’re on a strict schedule, space out cannabis and your depressant by at least four hours. But even this isn’t foolproof.
- Use CBD-dominant products. If anxiety or pain is your goal, look for products with CBD:THC ratios above 20:1. Early research shows these have far fewer interaction risks.
- Know the signs of overdose. Extreme drowsiness, slurred speech, slow or shallow breathing, confusion, inability to wake up-these aren’t "just high" symptoms. They’re medical emergencies.
What’s Being Done About It
Health systems are finally catching up. The National Institutes of Health poured $142.7 million into cannabis interaction research in 2023-up from under $30 million in 2020. Scientists are now developing risk-scoring tools that assign points based on THC strength, depressant type, and patient age. A score above 7 means high risk-and doctors are being told to find alternatives.Some states are moving toward mandatory screening. The American College of Physicians wants all medical cannabis programs to require interaction checks by 2025. That could prevent 2,300 ER visits a year.
For now, the message is clear: if you’re taking something to help you sleep, calm down, or manage pain, and you’re also using cannabis, you’re playing Russian roulette with your breathing. The odds are getting worse, not better.
Is There Any Safe Way?
There’s no guaranteed safe way to combine cannabis with CNS depressants. The only truly safe approach is to avoid the combination entirely.But if you’re on a prescription depressant and your doctor says cannabis might help, work with them to find alternatives. Could you switch to a non-sedating pain reliever? Could you try non-pharmacological therapies like physical therapy, cognitive behavioral therapy, or acupuncture? Could you reduce your depressant dose under supervision while slowly introducing low-dose CBD?
Some chronic pain patients have successfully cut their opioid use by nearly half while using low-dose THC under strict medical oversight. But that’s not a DIY project. It took a team of doctors, careful monitoring, and regular blood tests.
Don’t gamble with your life because you think you "know your body." The science is clear: when cannabis meets a CNS depressant, your body doesn’t know how to handle it. And your brain doesn’t realize how much it’s shutting down until it’s too late.

Josh Kenna
January 20, 2026 AT 10:25Man, I thought I was being smart mixing my Xanax with a little vape to chill out-turns out I was just one breath away from a body bag. That Reddit story about the 82% oxygen? That’s me last winter. Never again. Thanks for the wake-up call.
Erwin Kodiat
January 21, 2026 AT 13:53Been using CBD oil for my back pain for two years now. Never touched THC. Honestly? Best decision I ever made. My doc never mentioned the risks either-guess they assume we all know. Guess not.
Christi Steinbeck
January 22, 2026 AT 09:00If you’re on sleep meds and thinking cannabis is a ‘natural’ fix, you’re not healing-you’re gambling. Your brain doesn’t care if it’s plant-based or pharmaceutical. It just knows it’s being suppressed. Stop romanticizing it.
sujit paul
January 24, 2026 AT 05:00Of course the FDA adds warnings now-after decades of suppression. The pharmaceutical industry feared cannabis because it disrupts their profit model. This is not science-it’s control disguised as safety. Wake up, sheeple.
Tracy Howard
January 25, 2026 AT 08:29Can we just admit that Americans treat cannabis like candy? In Canada, we have regulated dosing, mandatory labeling, and doctors who actually talk to patients. You people treat medical advice like a TikTok trend. Disgraceful.
Jackson Doughart
January 26, 2026 AT 13:51I’ve been a nurse for 18 years. I’ve seen the aftermath-elderly patients found unresponsive after combining opioids, benzodiazepines, and ‘just a little edible.’ No one ever admits to using cannabis until it’s too late. The silence kills more than the drugs. Please, if you’re doing this, tell your provider. It’s not judgment-it’s survival.
Jake Rudin
January 27, 2026 AT 20:33It’s fascinating-THC binds to CB1 receptors, which are densely concentrated in the brainstem, the very region responsible for respiratory drive... and when you layer on GABAergic agents like benzodiazepines-whose binding sites overlap functionally, if not structurally-you create a pharmacological cascade that bypasses homeostatic feedback loops entirely... This isn’t synergy-it’s systemic override.
Lydia H.
January 28, 2026 AT 21:04I used to smoke every night with my muscle relaxer-thought it helped me sleep deeper. Turns out I was just drugging myself into a fog. I switched to CBD-only gummies, started therapy, and now I sleep better without any of it. You don’t need chemicals to rest. You just need to listen.
Valerie DeLoach
January 30, 2026 AT 11:49For anyone reading this who’s scared to talk to their doctor: you’re not alone. But your silence won’t protect you-it’ll endanger you. I’m a geriatric care coordinator. I’ve had three patients in the last year who nearly died from this exact combo. All of them said, ‘I didn’t think it was a big deal.’ It is. Please, speak up. Someone’s life depends on it.
Lewis Yeaple
January 31, 2026 AT 03:35According to the CDC’s 2023 National Poison Data System, 68% of cannabis-related ER visits involving CNS depressants occurred in patients aged 55–74. The mean THC concentration in those products was 19.3%. The mean concurrent benzodiazepine dose was 1.2 mg alprazolam equivalents. These are not anecdotes-they are epidemiological trends with statistical significance (p < 0.001).
Malikah Rajap
February 1, 2026 AT 19:41So… you’re saying I can’t chill with my weed and my Ativan? But… it’s the only thing that makes me feel normal. What if I just use one puff? And only at night? And never with alcohol? Isn’t that… enough? Please tell me I’m not crazy for needing this.