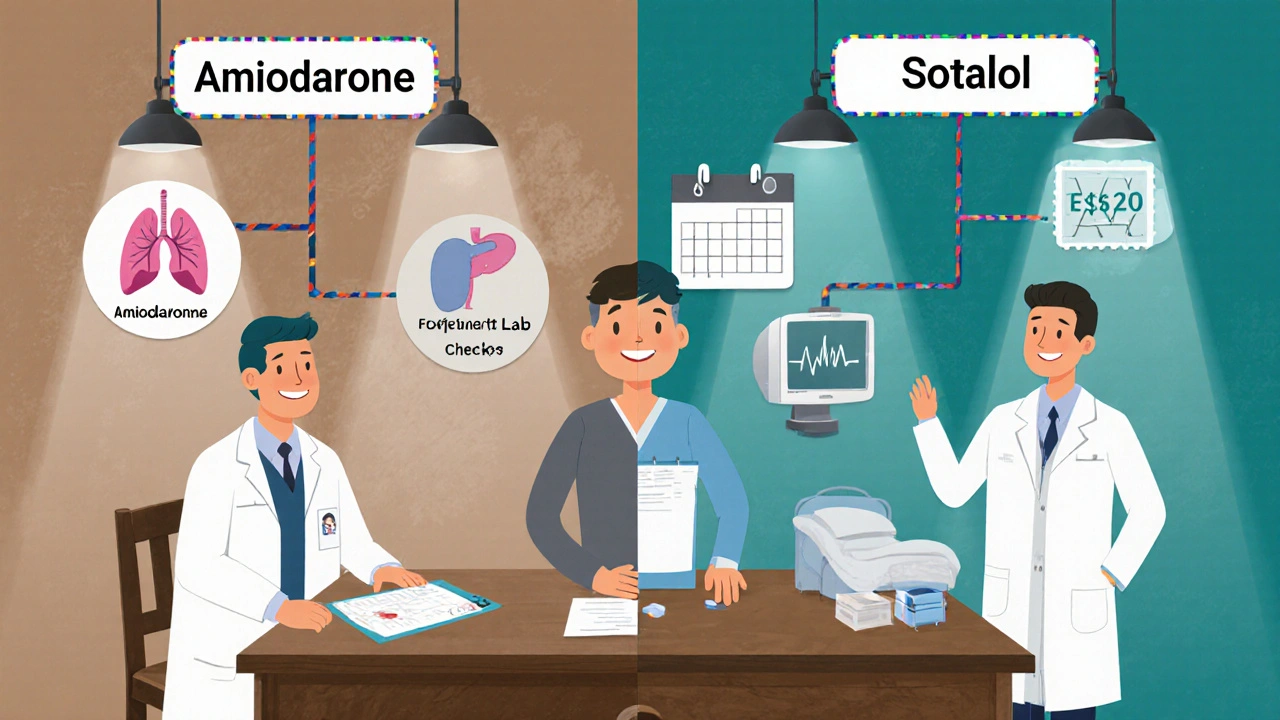
Amiodarone vs Sotalol Decision Aid
Select Patient Factors
Treatment Recommendation
Key Takeaways
- Amiodarone is highly effective for both ventricular and supraventricular arrhythmias but carries a broad side‑effect profile that often limits long‑term use.
- Sotalol combines class III potassium‑channel blockade with beta‑blocking activity, making it a solid option for atrial fibrillation and certain ventricular tachycardias, yet it demands strict QT monitoring.
- Choosing between the two hinges on the specific arrhythmia type, comorbid conditions, renal function, and the patient’s ability to tolerate monitoring.
- Both drugs interact with CYP3A4 enzymes; dose adjustments may be needed when used with common antihypertensives or antifungals.
- Cost considerations vary by region; in Australia, amiodarone is generally less expensive per tablet but may incur higher long‑term monitoring costs.
What Are Amiodarone and Sotalol?
When we talk about antiarrhythmic therapy, two names dominate the conversation: Amiodarone is a class III antiarrhythmic that blocks potassium channels, slows conduction, and has beta‑blocking and calcium‑channel effects. First approved by the FDA in 1985, it’s often the go‑to drug for refractory ventricular tachycardia and atrial fibrillation. Its sister drug, Sotalol combines class III potassium‑channel blockade with non‑selective beta‑adrenergic antagonism, making it useful for both atrial and ventricular arrhythmias. Sotalol entered the market in the early 1990s and is prized for its dual mechanism, especially in patients who need rate control alongside rhythm stabilization.
Mechanisms of Action - How They Work Differently
Both drugs prolong the cardiac action potential, but they get there via distinct pathways.
- Amiodarone: Primarily blocks the rapid component of the delayed rectifier potassium current (IKr), extending repolarization. It also blocks Na⁺ channels (class I effect), L‑type Ca²⁺ channels (class IV), and non‑selectively antagonizes β‑adrenergic receptors (class II). This multi‑modal profile explains its potency across a wide range of arrhythmias.
- Sotalol: Inhibits IKr similarly, but its beta‑blocking effect is the real differentiator. By reducing sympathetic tone, it lowers heart rate and myocardial oxygen demand, which helps prevent tachy‑arrhythmias triggered by stress.
The overlap in potassium‑channel blockade means both agents can cause QT interval prolongation, but the beta‑blockade in sotalol often tempers the pro‑arrhythmic risk compared with amiodarone’s broader receptor engagement.
Indications - When to Use Which
Guidelines from the American Heart Association (AHA) and the European Society of Cardiology (ESC) list specific scenarios.
| Condition | Amiodarone | Sotalol |
|---|---|---|
| Ventricular tachycardia (VT) - stable | First‑line for refractory VT | Alternative when EF > 35% and renal function adequate |
| Ventricular fibrillation (VF) - out‑of‑hospital | Adjunct to defibrillation | Not routinely used |
| Atrial fibrillation (AF) - rate‑control failure | Effective for cardioversion and maintenance | Effective for maintenance, especially in patients with concurrent hypertension |
| Supraventricular tachycardia (SVT) | Used when cathether ablation not possible | Limited role |
| Patients with reduced ejection fraction (EF ≤ 35%) | Preferred due to lower pro‑arrhythmic risk | Cautious use; monitor QT closely |
In practice, amiodarone becomes the rescue drug for life‑threatening VT or AF that doesn’t respond to other agents. Sotalol shines in patients who need both rhythm control and beta‑blockade, such as those with hypertension or ischemic heart disease.
Dosage & Administration - Practical Details
Both drugs have loading phases followed by maintenance dosing, but the schedules differ markedly.
- Amiodarone:
- Loading: 800-1200mg/day for 1week, then 400-600mg/day for 1week.
- Maintenance: 100-200mg/day, adjusted to plasma level (1-2.5µg/mL).
- Oral tablets are 200mg; IV formulation (150mg in 100mL D5W) is used for acute settings.
- Sotalol:
- Loading: 80mg PO twice daily for 3days.
- Maintenance: 80-160mg PO twice daily, titrated to QT interval (<500ms) and renal function (dose reduce if CrCl < 50mL/min).
- IV sotalol is rarely used; oral route dominates.
Renal clearance is the limiting factor for sotalol, whereas amiodarone’s long half‑life (≈58days) means steady‑state is reached only after weeks. This pharmacokinetic difference explains why amiodarone requires more intensive long‑term monitoring.
Side‑Effect Profiles - What to Watch For
Side‑effects are the biggest deal‑breaker for both agents, and they differ in organ system involvement.
| Adverse Effect | Amiodarone | Sotalol |
|---|---|---|
| Thyroid dysfunction | Hypo‑ or hyper‑thyroidism (10-15% incidence) | Rare |
| Pulmonary toxicity | Interstitial pneumonitis, fibrosis (5% risk) | None |
| Skin discoloration | Blue‑gray skin, photosensitivity | None |
| QT prolongation / Torsades | Occasional, dose‑dependent | Higher incidence, especially with hypokalaemia |
| Bradycardia | Common during loading | Common due to beta‑blockade |
| Drug interactions | Strong CYP3A4 inhibitor/inducer; interacts with warfarin, digoxin | Moderate CYP2C9 substrate; interacts with quinidine, certain antifungals |
Because amiodarone distributes into adipose tissue, side‑effects can appear months after discontinuation. Sotalol’s toxicity tends to be acute and reversible if the drug is stopped early.
Monitoring Requirements - Labs and ECG
Both drugs demand regular check‑ups, but the frequency and scope vary.
- Amiodarone:
- Baseline ECG, thyroid function tests (TSH, free T4), liver enzymes (ALT, AST), and chest X‑ray.
- Follow‑up: ECG & labs every 3months for the first year, then twice yearly.
- Pulmonary function tests if respiratory symptoms develop.
- Sotalol:
- Baseline ECG and serum electrolytes (K⁺, Mg²⁺).
- In‑hospital initiation (≥3days) with telemetry to monitor QT.
- Outpatient ECG at 1week, then monthly for the first 3months, then every 6months.
- Renal function every 6months; adjust dose accordingly.
Missing a QT check on sotalol can be fatal, especially in patients on diuretics. Amiodarone’s liver and thyroid surveillance is non‑negotiable because organ damage can be irreversible.
Cost and Accessibility - What Patients Pay
In Australia, the Pharmaceutical Benefits Scheme (PBS) lists amiodarone under a general subsidy, making a 200mg tablet cost roughly AU$0.85. Sotalol, also PBS‑listed, runs a similar price per 80mg tablet. However, the hidden costs differ:
- Amiodarone: Frequent lab work, imaging, and potential specialist referrals for pulmonary or thyroid issues can add AU$500-$800 per year.
- Sotalol: Initial inpatient monitoring (2-3days) adds AU$2,000-$3,000, but long‑term lab costs are lower (mainly electrolytes and renal function).
Insurance coverage typically absorbs the drug price but not the ancillary monitoring. For patients with limited access to labs, sotalol’s simpler follow‑up may be more affordable overall.
Decision‑Making Framework - Choosing the Right Drug
Below is a quick decision tree you can use during a clinic visit:
- Identify the primary arrhythmia type.
- Ventricular tachycardia or fibrillation → Consider amiodarone first.
- Atrial fibrillation with hypertension or ischemia → Lean toward sotalol.
- Assess comorbidities.
- Thyroid disease, lung disease, or liver impairment → Prefer sotalol.
- Renal insufficiency (CrCl < 30mL/min) → Avoid sotalol; amiodarone is safer.
- Review medication list for CYP interactions.
- Concomitant warfarin, digoxin, or certain antibiotics → Amiodarone may need dose adjustment.
- Concurrent quinidine or other QT‑prolonging drugs → Sotalol risk rises.
- Determine patient willingness for monitoring.
- Willing to attend frequent labs → Amiodarone acceptable.
- Prefers fewer visits, can handle brief hospitalization → Sotalol fits.
Always involve the patient in shared decision‑making. Explain that while amiodarone is a “strong but messy” option, sotalol is “clean but requires vigilant QT checks.”
Special Populations - Pregnancy, Children, and the Elderly
Data are limited for both drugs, but trends are clear:
- Pregnancy: Amiodarone is classified as Category D (evidence of fetal risk). Sotalol is Category C; it crosses the placenta and may cause fetal bradycardia.
- Pediatrics: Amiodarone is used for congenital long‑QT syndrome and refractory VT, dosed by weight (5-10mg/kg/day). Sotalol is approved for pediatric atrial fibrillation in doses 1-2mg/kg BID.
- Elderly (>75 years): Reduced renal clearance makes sotalol dosing tricky; amiodarone’s tissue accumulation can worsen pre‑existing lung disease common in this age group.
In each case, a cardiology consultation is advisable before initiating therapy.
Future Directions - Newer Alternatives and Ongoing Research
While amiodarone and sotalol remain staples, several newer agents are emerging:
- Dofetilide: Pure class III blocker, less organ toxicity but still needs inpatient initiation.
- Vernakalant: Atrial‑selective agent showing promise in rapid conversion of AF with minimal QT effects.
- Cardiac ablation technology: Advances in cryo‑ablation now rival drug therapy for many AF patients, reducing the need for long‑term antiarrhythmics.
Until these become widely accessible, clinicians will continue to weigh amiodarone against sotalol based on the factors outlined above.
Frequently Asked Questions
Can I switch from amiodarone to sotalol safely?
A gradual taper of amiodarone over several weeks is recommended to avoid rebound arrhythmias. After the plasma level falls below 1µg/mL, sotalol can be introduced with a 3‑day in‑hospital QT monitoring phase.
Why does amiodarone cause lung problems?
Amiodarone’s high iodine content and lipophilicity lead to phospholipid accumulation in alveolar macrophages, triggering an inflammatory response that can progress to fibrosis if not caught early.
What electrolyte levels are critical before starting sotalol?
Maintain potassium >4.0mmol/L and magnesium >2.0mg/dL. Low levels markedly increase the risk of torsades de pointes when sotalol lengthens the QT interval.
Is there a generic version of sotalol?
Yes, generic sotalol is available in most pharmacies and is covered by the Australian PBS, making it cost‑comparable to brand‑name.
How often should thyroid function be checked on amiodarone?
Baseline, then at 3 months, 6 months, and annually thereafter. Any symptoms of hyper‑ or hypothyroidism warrant an immediate test.

Gail Hooks
October 15, 2025 AT 17:57Wow, the depth of this comparison really makes you think about how we balance efficacy and safety in cardiology 🌟. Amiodarone’s broad spectrum is impressive, but the side‑effect baggage can be a nightmare for patients 😅. Sotalol’s dual action feels like a smart compromise for many with hypertension and AF. It's fascinating how pharmacogenomics might soon help us predict which drug fits best for an individual. Ultimately, shared decision‑making should guide the choice, with close monitoring on both sides. 💡
Derek Dodge
October 27, 2025 AT 20:37I think sotalol is easier to manage.
AARON KEYS
November 9, 2025 AT 00:17While both agents have their place, it’s worth noting that the ESC guidelines specifically recommend amiodarone for refractory ventricular tachycardia when structural heart disease is present, whereas sotalol is generally reserved for patients with preserved ejection fraction and adequate renal function. The nuance lies in the monitoring requirements: amiodarone demands thyroid and pulmonary surveillance, while sotalol calls for meticulous QT interval tracking, especially in the elderly.
Summer Medina
November 21, 2025 AT 03:57Let me tell you why amiodarone is the real champion for arrhythmia control, and why any other drug is just a second‑rate wannabe. First, it attacks the heart’s electrical system from every angle – potassium, sodium, calcium, even beta receptors – that’s why it works on almost every scar‑red rhythm out there. Second, the side‑effects are a price you pay for power, so stop whining about lung fibrosis or thyroid storms when you’re staring down a ventricular storm that could kill you. Third, the cost is nothing compared to the ICU time you’d waste chasing a sotalol‑induced torsade that could have been avoided with a solid amiodarone load. Fourth, the dosage flexibility lets you tailor therapy from a massive loading phase down to a gentle maintenance that keeps the rhythm in check without constant hospital visits. Fifth, the long half‑life means you’re not missing doses every other day – you get steady state and stable electrophysiology. Sixth, you don’t need to worry about renal clearance like you do with sotalol, which can be disastrous in patients with borderline kidney function. Seventh, the data from multiple randomized trials consistently show lower mortality with amiodarone in severe heart failure compared to other class III agents. Eighth, the drug’s lipophilic nature means it gets into cardiac tissue better than sotalol ever could, giving it a more profound effect on refractory arrhythmias. Ninth, the international guidelines still list amiodarone as first‑line for refractory VT and VF – that’s not a coincidence, that’s evidence. Tenth, you can give it IV in emergencies, something you can’t do with sotalol, and that alone saves lives on the defibrillator. Eleventh, the monitoring schedule, while intensive, is well‑established and can be handled by any competent cardiology team. Twelfth, let’s not forget the patient’s perspective – many prefer a single drug rather than juggling multiple agents with unpredictable interactions. Thirteenth, the pharmaceutical community has spent decades refining amiodarone formulations to reduce toxicity, a testament to its importance. Fourteenth, the drug’s cost per tablet may be lower in many regions, even after factoring in lab work, because you avoid repeated hospital admissions for sotalol‑induced arrhythmias. Fifteenth, the simple truth is that amiodarone works, and if you’re looking for a drug that will actually stop a life‑threatening rhythm, you grab amiodarone and you run with it. Anything else is just a compromise that most clinicians can’t afford in real‑world practice.
Melissa Shore
December 3, 2025 AT 07:37When you look at the practical side of prescribing amiodarone versus sotalol you have to weigh not only the pharmacology but also the logistics of follow‑up. Amiodarone’s need for thyroid and liver panels every few months can feel burdensome, yet those labs are usually drawn alongside routine heart failure checks, making the workflow smoother. Sotalol, on the other hand, forces you into a strict QT surveillance protocol after every dose adjustment – a process that can tie up clinic slots and require patients to stay in the hospital for 48‑hour telemetry. In many outpatient settings the ability to schedule that telemetry window is limited, pushing clinicians toward the drug with less intensive immediate monitoring. Cost is another factor; while amiodarone pills may be cheaper per unit, the cumulative expense of specialty labs can add up, whereas sotalol’s generic nature often appears attractive on the pharmacy bill. Ultimately the decision rests on patient‑specific variables – renal function, baseline QT, co‑medications that affect CYP3A4 – and the health system’s capacity to support the required surveillance without causing delays in care.
Michelle Pellin
December 15, 2025 AT 11:17In the grand theater of cardiac therapeutics, amiodarone assumes the role of the seasoned virtuoso, commanding the stage with a repertoire that spans ventricular and supraventricular domains alike. Its multifaceted mechanism, akin to a symphony of ion‑channel modulation, delivers a performance that few rivals can match. Yet, as with any dramatic masterpiece, the curtain rises on a poignant intermezzo of adverse effects – pulmonary fibrosis, thyroid dysfunction, and hepatic derangements – demanding vigilant oversight. Sotalol, while perhaps less flamboyant, offers a refined duet of potassium‑channel blockade and beta‑adrenergic antagonism, striking a harmonious chord in patients where rate control is paramount. The choreography of dosing, monitoring, and patient selection thus becomes an elegant ballet, wherein clinicians must balance efficacy with safety, cost with convenience, and tradition with innovation.
Keiber Marquez
December 27, 2025 AT 14:57Amiodaron is just better for fatal arrithmia.
Lily Saeli
January 8, 2026 AT 18:37It’s morally indefensible to prescribe a drug that could damage the lungs and thyroid when a safer alternative exists, even if it requires a bit more monitoring. Patients deserve treatment that respects their long‑term health, not just a quick fix that could compromise organ function.
Joshua Brown
January 20, 2026 AT 22:17For clinicians looking to optimise therapy, consider the following practical checklist: first, assess renal function – if eGFR is below 50 mL/min, amiodarone is generally safer than sotalol; second, review baseline electrolytes – maintain potassium >4.0 mmol/L and magnesium >2.0 mg/dL to mitigate QT‑prolongation risks; third, schedule thyroid and pulmonary function tests at baseline, 3 months, 6 months, then annually for amiodarone patients; fourth, arrange a 48‑hour telemetry admission when initiating sotalol to monitor QT interval closely; fifth, educate patients on symptoms of thyroid dysfunction and pulmonary toxicity, encouraging prompt reporting; sixth, consider drug‑interaction screening, especially with CYP3A4 inhibitors, which can elevate plasma levels of both agents; seventh, document all monitoring results in the electronic health record with alerts for overdue labs; eighth, involve a multidisciplinary team – cardiology, pharmacy, and primary care – to coordinate follow‑up; ninth, weigh cost‑effectiveness – while amiodarone tablets may be cheaper, the downstream monitoring expenses can offset the savings; tenth, reassess therapy regularly, aiming for the lowest effective dose to reduce toxicity risk.
Meg Mackenzie
February 2, 2026 AT 01:57There’s a hidden agenda behind the way these drugs are marketed. Companies push sotalol as the “clean” option, but they downplay the long‑term cardiac remodeling risks that only become apparent after years of use. Meanwhile, amiodarone’s side‑effects are well documented, but the narrative suggests it’s just a “last resort,” framing the truth to keep patients from demanding more transparent research. It’s all about profit, not patient safety.
Madeline Leech
February 14, 2026 AT 05:37Listen up, the data is crystal clear – amiodarone beats sotalol in most high‑risk cases and anyone who says otherwise is just ignoring the evidence. If you’re not on amiodarone for refractory VT, you’re doing your patient a disservice.