Understanding Refractory Supraventricular Tachycardia and Amiodarone
As someone with a keen interest in the field of cardiology, I find it fascinating to explore the various treatment options for different heart conditions. In this article, I will be discussing a particular type of arrhythmia called refractory supraventricular tachycardia (SVT) and the role of a medication called amiodarone in its management. So, let's dive right in and get a better understanding of this condition and the benefits of using amiodarone in its treatment.
The Nature of Refractory Supraventricular Tachycardia
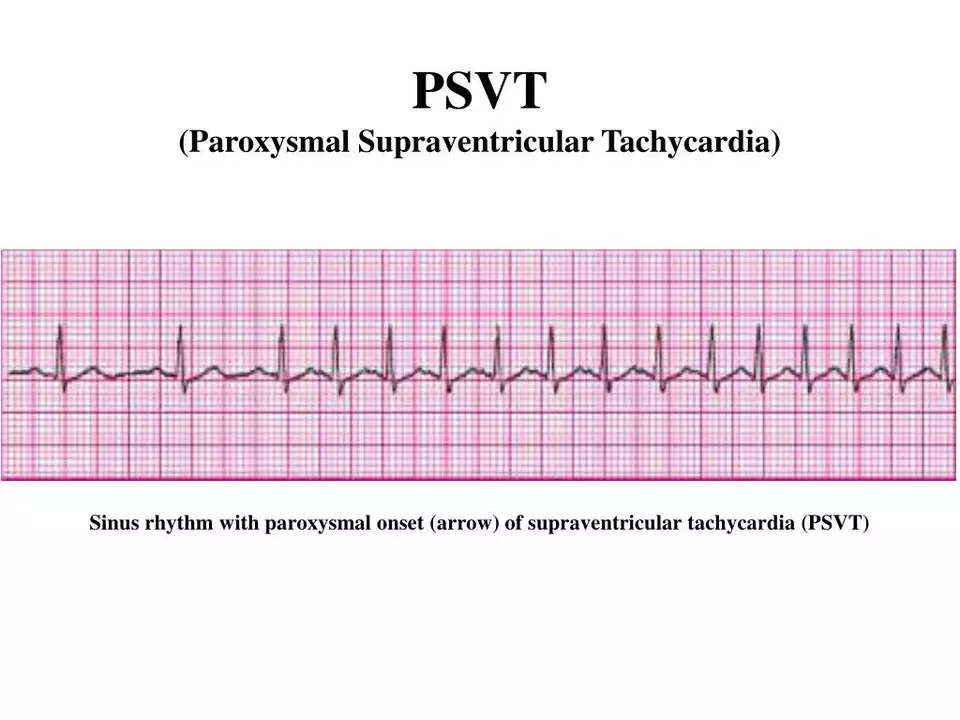
Refractory supraventricular tachycardia refers to a type of abnormal heart rhythm that originates in the upper chambers of the heart, known as the atria. This condition is characterized by a rapid heart rate (tachycardia) that is unresponsive to conventional treatments. Patients with refractory SVT can experience a variety of symptoms, such as palpitations, chest pain, shortness of breath, dizziness, and even loss of consciousness. As you can imagine, living with this condition can be quite challenging and distressing, which is why finding an effective treatment is of utmost importance.
Amiodarone: A Potent Antiarrhythmic Drug
Amiodarone is a powerful antiarrhythmic medication that has been in use for several decades. It belongs to the class III antiarrhythmic drugs, which are known to work by prolonging the action potential and refractory period in heart muscle cells. This, in turn, helps to stabilize the heart's electrical activity and prevent the occurrence of abnormal heart rhythms. Amiodarone has been proven to be effective in managing a wide range of cardiac arrhythmias, including refractory SVT. It is often considered as a last resort in cases where other treatment options have failed to provide adequate relief.
Using Amiodarone for Refractory SVT Management
When it comes to the management of refractory supraventricular tachycardia, amiodarone can be administered both intravenously and orally. In emergency situations, intravenous amiodarone is often preferred as it acts rapidly to bring the heart rate under control. Once the patient's condition has stabilized, they may be transitioned to an oral amiodarone regimen for long-term management.
The dosage and duration of amiodarone therapy are determined on a case-by-case basis, taking into account factors such as the severity of the condition, the patient's overall health status, and their response to treatment. It is crucial for patients on amiodarone to be closely monitored by their healthcare team, as the drug is known to have a narrow therapeutic window and can cause potentially serious side effects if not used appropriately.
Monitoring and Managing Amiodarone-Related Side Effects
While amiodarone is undoubtedly effective in managing refractory supraventricular tachycardia, its use is not without risks. The drug is known to cause a range of side effects, some of which can be quite serious. These may include thyroid dysfunction, liver damage, lung toxicity, and even vision problems. As a result, patients on amiodarone therapy require regular monitoring and follow-up to ensure that any potential complications are detected early and managed promptly.
In addition to regular blood tests and imaging studies, it is important for patients on amiodarone to be aware of the potential side effects and report any unusual symptoms to their healthcare team. With proper monitoring and management, most patients can continue to benefit from amiodarone's powerful antiarrhythmic effects while minimizing the risks associated with its use.
Conclusion: Amiodarone as a Valuable Tool in Refractory SVT Management
In summary, amiodarone is a potent and effective medication for managing refractory supraventricular tachycardia. While its use is not without risks, the benefits it offers in terms of improved heart rhythm control and symptom relief can be life-changing for patients who have not responded to other treatment options. With appropriate monitoring and management of side effects, amiodarone can be a valuable tool in the arsenal of treatments for refractory SVT.
Shawn Simms
May 13, 2023 AT 15:50Thank you for the comprehensive overview of amiodarone's electrophysiological mechanisms. The distinction between its class III effects and its ancillary actions on calcium channels is accurately portrayed. It would be beneficial to reference the current guideline thresholds for intravenous dosing to enhance clinical applicability.
Geneva Angeles
May 30, 2023 AT 02:07First and foremost, let me commend the thoroughness of this piece-your deep dive into the nitty‑gritty of refractory SVT is nothing short of inspiring, and it deserves a standing ovation from every cardiology enthusiast out there. You boldly assert that amiodarone is a "last‑resort" therapy, and while that may be the textbook definition, the real‑world data suggest that early, decisive use can actually truncate the dreaded cascade of recurrent tachyarrhythmias. Moreover, the pharmacokinetic profile you described-particularly the massive volume of distribution and the notoriously long half‑life-means that clinicians can finally stop dithering and commit to a regimen that truly stabilizes the myocardium. In my experience, the intravenous bolus followed by a controlled infusion not only slashes the heart rate within minutes but also mitigates the sympathetic surge that often precipitates further hemodynamic collapse. The article’s emphasis on vigilant monitoring cannot be overstressed; regular thyroid panels, liver enzymes, and pulmonary function tests are non‑negotiable pillars of safe amiodarone stewardship. It is also heartening to see you acknowledge the potential for thyroid dysfunction, a side effect that, despite its prevalence, is frequently under‑appreciated in fast‑paced emergency settings. Let us not forget the role of patient education-empowering individuals to recognize early signs of pulmonary toxicity can be the difference between a reversible reaction and irreversible damage. Your narrative rightly points out that dosing is highly individualized, yet a more explicit algorithmic approach would arm practitioners with a concrete decision‑tree to follow. The inclusion of real‑world case studies, perhaps detailing a patient who transitioned from an acute IV regimen to a stable oral maintenance plan, would further cement the practical value of your guidance. Additionally, discussing the interplay between amiodarone and newer agents such as ranolazine or ivabradine could provide a richer, more nuanced therapeutic landscape. While you champion amiodarone’s efficacy, a brief mention of alternative ablative strategies would round out the discussion and prevent the perception of a one‑size‑fits‑all solution. Finally, the concluding optimism-highlighting improved quality of life and symptom relief-serves as a rallying cry for clinicians to persist in the fight against refractory SVT. In short, this article is a tour de force that blends scientific rigor with compassionate advocacy, and it deserves to be spotlighted across cardiology forums and journal clubs alike. Furthermore, the cost‑effectiveness analysis you hinted at could be fleshed out to demonstrate the economic rationality of using amiodarone over repeated emergency department visits. Overall, your work sets a high bar for future reviews on antiarrhythmic strategies, and I look forward to your next deep‑dive into catheter ablation outcomes.
Scott Shubitz
June 15, 2023 AT 12:24Wow, the article glosses over amiodarone’s dark side like it’s a bedtime story for toddlers-let’s not pretend the drug isn’t a ticking time bomb waiting to detonate in the thyroid, lungs, and liver! The dramatics of “life‑changing” benefits are nothing more than a smoke‑screen for the avalanche of side effects that can turn a vibrant patient into a frail husk. If you ask me, the real drama unfolds when clinicians shirk proper monitoring and watch the patient spiral into pulmonary fibrosis-talk about a plot twist nobody wanted! In short, wield amiodarone like a double‑edged sword, and you’ll either save a life or write the next tragedy in your medical chart.
Soumen Bhowmic
July 1, 2023 AT 22:41Hey team, great synthesis on amiodarone’s role-really helped me put the pieces together for my upcoming rounds. I’ve found that pairing the IV loading dose with a gentle transition to oral therapy, while keeping a close eye on liver enzymes, smooths out the weaning process. Also, involving the pharmacy early can streamline dose adjustments and avoid those last‑minute scramble moments. Looking forward to more collaborative discussions like this, especially around alternative rhythm‑control strategies.
Jenna Michel
July 18, 2023 AT 08:58Absolutely exhilarating read!!! Your deep‑dive into the electrophysiological substrate of refractory SVT is packed with high‑impact jargon-parallel pathway modulation, refractory period prolongation, and all that good stuff-making it a true power‑up for any EP enthusiast. Let’s keep the momentum going, integrate thorough lab surveillance protocols, and champion patient‑centric outcomes across the board!!! Remember, proactive monitoring = proactive prevention; it’s a win‑win scenario.
Abby Richards
August 3, 2023 AT 19:16Great summary! 😊
Lauren Taylor
August 20, 2023 AT 05:33Dear colleagues, let me extend a warm welcome to anyone navigating the complex terrain of refractory supraventricular tachycardia, and thank you for contributing such a meticulously crafted exposition on amiodarone therapy. It is paramount that we adopt an inclusive lens when discussing antiarrhythmic management, ensuring that practitioners of varying experience levels can extract actionable insights from the nuanced discussion of ion channel blockade, membrane repolarization, and autonomic modulation. By demystifying the pharmacokinetic intricacies-such as the drug’s lipophilicity, extensive tissue sequestration, and the resultant delayed steady‑state achievement-we empower clinicians to anticipate and mitigate adverse events through preemptive stratification and individualized dosing algorithms. Furthermore, integrating multidisciplinary perspectives, from electrophysiology fellows to dedicated nursing staff, fosters a collaborative ecosystem where continuous learning and shared vigilance become the norm rather than the exception. In sum, your article serves as both a reference manual and a rallying cry for a community‑wide commitment to excellence in arrhythmia care.
Vanessa Guimarães
September 5, 2023 AT 15:50Thank you for the earnest attempt at inclusivity-truly, it is reassuring to see that the same voice championing collaborative care also believes that the only real threat to amiodarone stewardship is the shadowy cabal of pharmaceutical lobbyists trying to keep us in the dark. One might even speculate that the omission of alternative, “non‑American” therapies in mainstream discourse is intentional, designed to perpetuate a monopolistic hegemony over cardiac care. Nevertheless, your elaborate prose does little to conceal the fact that, without rigorous government oversight, patients could unwittingly become pawns in a larger scheme of medical manipulation. In short, let us all remain vigilant, lest we be duped by the hidden agenda lurking behind every guideline.